| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://gr.elmerpub.com/ |
Original Article
Volume 000, Number 000, November 2024, pages 000-000
Think With Your Gut: A Retrospective Analysis on the Effects of Chronic Gastrointestinal Illness and Psychiatric Comorbidities
Rakahn Haddadina, e, Danny Aboujamrab, Zachary I. Merhavyc, George Tradd, John Ryand, Kartika Shettya
aDepartment of Internal Medicine, HCA Healthcare; MountainView Hospital, Las Vegas, NV, USA
bDepartment of Internal Medicine, Medical University of South Carolina (MUSC) Health Florence, SC, USA, Florence, SC 29505, USA
cDepartment of Clinical Sciences, Ross University School of Medicine, Pontiac, MI 48341, USA
dDepartment of Gastroenterology, HCA Healthcare; Southern Hills Hospital, Las Vegas, NV 89128, USA
eCorresponding Author: Rakahn Haddadin, Department of Internal Medicine, HCA Healthcare; MountainView Hospital, Las Vegas, NV 89128, USA
Manuscript submitted August 2, 2024, accepted September 30, 2024, published online November 13, 2024
Short title: Chronic GI Illness and Psychiatric Comorbidities
doi: https://doi.org/10.14740/gr1765
| Abstract | ▴Top |
Background: As mental health awareness increases, healthcare professionals must understand the interplay between chronic gastrointestinal (GI) conditions and psychological well-being, particularly regarding healthcare utilization. This study uniquely aggregates various chronic GI disorders, such as inflammatory bowel disease, celiac disease, and eosinophilic esophagitis, to examine their impact on depression and anxiety.
Methods: Utilizing a retrospective observational design, we analyzed data from 34,876 patients admitted to HCA national hospitals from January 2016 to December 2022.
Results: We found that patients with GI conditions and comorbid psychiatric disorders had significantly higher readmission rates and longer hospital stays compared to those without mental health diagnoses. Results indicated that patients with GI disorders and depression or anxiety were 1.29 times more likely to be readmitted within 90 days and had 1.50 times longer hospital stay.
Conclusion: These findings underscore the importance of integrated care approaches addressing physical and mental health in managing chronic GI conditions. Future research should focus on targeted interventions to enhance mental health management and improve outcomes in this vulnerable patient population.
Keywords: Gastrointestinal conditions; Mental health; Gastroesophageal reflux disease; Diverticulosis; Inflammatory bowel disease
| Introduction | ▴Top |
As the topic of mental health and resources for mental health increases, healthcare professionals need to understand better how these conditions affect their patients, as they can be debilitating and cause an increase in healthcare utilization [1, 2]. Although previous studies have examined healthcare outcomes for specific gastrointestinal (GI) issues, this study stands out by aggregating and individualizing various chronic GI conditions to provide a more comprehensive overall picture of their potential mental health exacerbation [3-5]. There is still a common misconception that psychological concerns in GI conditions only relate to disorders of gut-brain interaction. Current research suggests there is significant and persistent psychological comorbidity among mood disorders in organic GI disorders, such as inflammatory bowel disease (IBD), celiac disease, and eosinophilic esophagitis [4, 5]. Understanding each specific GI condition in this context underscores the importance of considering psychological factors and how one may evaluate and manage each disease [4]. Having different physical illnesses, symptoms, and treatment plans may all be distressing in their own way and cause distorted thinking, maladaptive coping, and other mood disturbances [4]. Sustained and acute life-threatening stressors can play an essential role in the onset and potential modulation of specific GI symptoms as well as in the development of affective disorders, such as depression, anxiety, and post-traumatic stress disorder (PTSD) [6]. Numerous factors play a role in the progression of GI conditions, such as a patient’s personality and coping style, past abuse and traumatic events, health beliefs and illness behaviors, and heredity. However, emotional stressors such as chronic stress, depression, and anxiety demonstrate the most substantial evidence for the progression of GI conditions [7-9]. Previous research has shown that gut microbiota responds to emotional stressors with one pathophysiologic mechanism through the effect of catecholamines on altering the growth, motility, and virulence of pathogenic and commensal bacteria, thereby influencing the outcome of infections and other GI disorders [9].
This study explores research findings on how the impact of a chronic GI condition can cause depression and/or anxiety. It compares it to a population without a diagnosis of depression and/or anxiety. Identifying relevant psychosocial factors in patients with these chronic GI disorders is essential for clinicians as it can drastically influence the flow of care and maybe a critical determinant of outcomes [10]. In some studies, many common GI disorders were found to be particularly prevalent in young adults who experience some level of chronic stress, depression, or anxiety [11-14]. As there continues to be a rise in understanding the relationship between these two comorbid conditions, it is crucial to pair the understanding of this relationship with the proper approach and management of these patients’ conditions [15]. By providing a comprehensive overview of the studies assessing these relationships, the impact of a GI condition on a psychiatric diagnosis can be better understood in hopes that it can drive further targeted management of these conditions. The outcomes assessed in this manuscript were length of stay and readmission, as these variables have not been looked at previously in these population groups.
| Materials and Methods | ▴Top |
A retrospective observational study was conducted on HCA national hospitals between January 2016 and December 2022. Patients met the inclusion criteria if they were > 18 years of age and admitted with a diagnosis of one or more of the following chronic GI conditions: lactose intolerance, celiac disease, malabsorption syndrome, gastroesophageal reflux disease (GERD), gastroparesis, diverticulosis, IBD, hemorrhoids, eosinophilic esophagitis, irritable bowel disease. Patients were excluded if they left against medical advice, were missing race and gender documentation, and had no GI diagnosis. Patients were then divided into a group with depression/anxiety and a group without depression/anxiety. Readmission was analyzed using logistic regression, and hospital length of stay was analyzed using a zero-inflated negative binomial regression. We sought to determine the effect of having a GI condition and depression/anxiety on the length of stay in days and readmission.
While not under direct investigation, variables influencing the listed outcomes were controlled, including age, race, gender, diabetes, hypertension, hyperlipidemia, and insurance type. Age was operationalized over the years, and race was self-reported as Black, Hispanic, White, or other. Gender was self-reported as female or male. Diabetes, hypertension, and hyperlipidemia were treated as dichotomous variables, and patients were categorized as either having or not having these diseases.
All control variables were obtained based on chart reviews pulled by HCA statisticians and gathered from patient-documented information or ICD-10 codes. This allowed us to parse out the effect of having a GI condition and depression/anxiety on the outcome variables over and above the controlled variables.
This project was exempted from IRB approval. This study was performed in compliance with IRB regarding research involving human subjects.
| Results | ▴Top |
A total of 34,876 patients were included in the study. Descriptive statistics of the patient population are presented in Table 1.
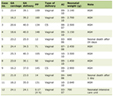 Click to view | Table 1. Patient Demographics |
Among patients with GI diagnoses at the index encounter, those with depression and/or anxiety were 1.29 more likely to be readmitted within 90 days when controlling for age, race, gender, diabetes, hypertension, and hyperlipidemia (P < 0.0001, 95% confidence interval (CI) 1.18 - 1.41). Diagnoses of depression and/or anxiety were significantly associated with an increase in hospital stay 1.50 (χ2 = 50.88, P < 0.0001, 95% CI 1.31 - 1.60).
Lactose intolerance, celiac disease, or malabsorption
A total of 485 patients with either lactose intolerance, celiac disease, or malabsorption syndrome were included in the study. The data showed that there was not an increase in readmission for patients with depression/anxiety in this population (P = 0.1304).
Eosinophilic esophagitis, gastritis, or colitis
A total of 450 patients with either eosinophilic esophagitis, gastritis, or colitis were included in the study. Patients diagnosed with depression or anxiety were significantly more likely (odds ratio (OR) = 2.63) to be readmitted within 90 days (P = 0.0101, 95% CI 1.26 - 5.49).
Diverticulosis and irritable bowel syndrome (IBS)
For this population, both diverticulosis (5,844 total patients) and IBS (837 total patients) did not show a difference in readmission in patients with a diagnosis of depression/anxiety (P = 0.712, P = 0.594, respectively).
GERD
A total of 22,460 patients with GERD were included in the study. Those diagnosed with depression and/or anxiety were 1.26 times as likely to be readmitted within 90 days compared to those not diagnosed with anxiety or depression (P < 0.0001, 95% CI 1.13 - 1.40).
| Discussion | ▴Top |
This study compared healthcare outcomes in patients with GI conditions, such as lactose intolerance, celiac disease, malabsorption syndrome, GERD, gastritis, diverticulosis, IBD, eosinophilic esophagitis, and IBS. Patients with these GI conditions were compared to those with and without a comorbidity of psychiatric conditions of depression or anxiety.
Current theories and the gut-brain axis influence
Numerous previous studies outline proposed mechanisms and theories as to why individuals with psychiatric conditions have higher rates of GI disorders, yet in studies such as the one presented, the mechanism for why the reverse is not fully understood. Many believe there is a possibility that those with GI conditions who later find out they have a psychiatric comorbidity may have previously been affected by the psychiatric condition without diagnosis, which is evidenced in specific patient groups with limited access to healthcare, those with a history of sexual, physical, or emotional abuse, those with food insecurities, or those in lower socioeconomic status (SES) classes [15].
Another theory is that individuals with an undiagnosed pre-existing affective disorder are more likely to present with healthcare-seeking behaviors, thus potentially serving as one contributing reason for higher rates of diagnosis of GI conditions among these populations [6]. Thirdly, it is assumed that individuals with chronic GI conditions are more likely to seek healthcare due to the frequency and severity of their symptoms [6].
In one population-based study, it was demonstrated that neuroticism, psychological comorbidity, and a history of abuse did not yield an explanation for healthcare-seeking behaviors. Still, the severity and duration of abdominal pain were shown to have statistically significant and independent effects on the probability of ever having sought GI care in the initial visit [16]. Another study delineated that GI symptom burden positively correlated with depressive symptom severity [12]. However, it has been shown that beyond the initial visit for individuals with chronic GI conditions, there is a positive correlation between the severity of GI symptoms and the prevalence of psychiatric diagnoses, such as depression and anxiety [6]. This aids in the understanding that psychological conditions are not part of chronic GI conditions but can influence the severity of symptoms, leading to more healthcare-seeking behaviors [6].
Harkening back to the changes in gut microbiota, there is clear evidence that suggests the gut microbiota influences the development of both GI and non-GI diseases [4]. Dysbiosis and inflammation have already been linked to several mental illnesses, including depression and anxiety [4, 17]. One study suggests that reducing alpha diversity may predispose individuals to inflammatory complications and infections [17]. The authors illustrated a decrease in alpha diversity, and a clear structural separation exists in the gut microbiota of immunodeficient mice compared to healthy mice [17]. The pathogenesis of certain chronic GI conditions is believed to involve an aberrant immune response to intestinal microbiota in genetically susceptible individuals [17]. Thus, this supports the hypothesis that if this dysbiosis occurs as a result of the mounted immune response, the individual is not only more susceptible to chronic GI conditions but to mental illnesses, such as depression and anxiety, as well.
Even with this foundational understanding and current theories, it is difficult to ascertain the exact reason why patients with chronic GI conditions are later diagnosed with depression and anxiety. Stress is one specific relationship thought to be bidirectional. Although life stresses and traumatic life events may influence the severity of GI symptoms, it is believed that the severity of GI symptoms can be considered life stressors themselves, leading to the development of psychiatric conditions over time [12]. The general thought is that exaggerated GI symptoms may cause a more significant impact on overall mood and psychiatric function in an otherwise healthy individual [12].
Readmission rates and length of stay
This study found a statistically significant difference in the readmission rates of patients with GI conditions and comorbid psychiatric conditions compared to those without psychiatric comorbidities. Patients with GI conditions, defined above, were 1.29 times more likely to have a readmission within 90 days compared to patients with GI conditions without a comorbid psychiatric condition. In addition to readmission, the study also analyzed the length of hospital duration. Patients with GI conditions concurrent with depression or anxiety were found to be associated with an increased length of stay. In patients with GI conditions comorbid with psychiatric conditions, they were 1.5 times more likely to experience a more extended hospital admission. These findings suggest that patients with GI conditions and comorbid psychiatric conditions are more likely to experience potential adverse healthcare outcomes requiring rehospitalization and increased hospitalization duration.
Lactose intolerance, celiac disease, or malabsorption
In our study of 485 patients with lactose intolerance, celiac disease, or malabsorption syndrome, we did not see an increase in readmission in those with a diagnosis of depression/anxiety; this can be due to the decrease in the severity of symptoms caused by lactose intolerance, celiac disease, or malabsorption syndrome.
Eosinophilic esophagitis, gastritis, or colitis
This study highlighted the significant impact of mental health diagnoses on readmission rates in patients with eosinophilic esophagitis, gastritis, or colitis. The findings suggest that patients with depression or anxiety are at a higher risk of readmission within 90 days. Early detection of these conditions may lead to better treatment adherence and follow-up [9]. This can be attributed to the distressing events and frequent hospitalizations that patients with these diagnoses have.
Diverticulosis and IBS
In both of these populations, there was no statistically significant association in readmission for patients with depression/anxiety. It is unclear why this is the cause, as patients with IBS have less symptom control. Future studies will need to evaluate these diagnoses further.
GERD
In our study, patients diagnosed with depression and/or anxiety had a significantly higher likelihood of readmission, highlighting the impact of mental health on the management and outcomes of GERD. This suggests a need for integrated care approaches addressing both physical and mental health to reduce readmission rates in this patient population.
Significance in future directions
This highlights the need for a multidisciplinary approach in managing patients with chronic GI conditions to optimize concurrent psychiatric conditions medically.
Diagnoses of depression and/or anxiety significantly increase the likelihood of 90-day readmission among GERD patients, even when controlling for age, race, gender, diabetes, hypertension, and hyperlipidemia. These findings suggest that mental health screening and management should be integral components of care for GERD patients to reduce readmission rates potentially. Future research should explore targeted interventions to address mental health issues in this population to improve overall patient outcomes and reduce healthcare costs.
Conclusions
The findings of our study highlight the need for targeted interventions that consider the numerous demographic and comorbid factors to reduce readmission rates within these patient populations. Mental health screening and management should be integral components of care for patients with chronic GI conditions to minimize readmission rates potentially. Future research should explore different methods to design targeted interventions to address mental health issues in this population better to reduce overall healthcare costs and ultimately improve patient outcomes.
Acknowledgments
None to declare.
Financial Disclosure
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of its author(s) and do not necessarily represent the official views of HCA Healthcare or any affiliated entities.
Conflict of Interest
All authors have no conflict of interest to declare.
Informed Consent
Not applicable.
Author Contributions
Rakahn Haddadin, Danny Aboujamra, Zachary I. Merhavy, George Trad, and John Ryan: conceived and designed the analysis, collected the data, contributed data or analysis tools, performed the analysis, and wrote the paper. Kartika Shetty: conceived and designed the analysis, collected the data, contributed data or analysis tools, and performed the analysis.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Wong JJ, Maddux M, Park KT. Mental health service needs in children and adolescents with inflammatory bowel disease and other chronic gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2018;67(3):314-317.
doi pubmed - Zhang AZ, Wang QC, Huang KM, Huang JG, Zhou CH, Sun FQ, Wang SW, et al. Prevalence of depression and anxiety in patients with chronic digestive system diseases: a multicenter epidemiological study. World J Gastroenterol. 2016;22(42):9437-9444.
doi pubmed pmc - Shah E, Rezaie A, Riddle M, Pimentel M. Psychological disorders in gastrointestinal disease: epiphenomenon, cause or consequence? Ann Gastroenterol. 2014;27(3):224-230.
pubmed pmc - Person H, Keefer L. Psychological comorbidity in gastrointestinal diseases: update on the brain-gut-microbiome axis. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110209.
doi pubmed pmc - Lee SP, Sung IK, Kim JH, Lee SY, Park HS, Shim CS. The effect of emotional stress and depression on the prevalence of digestive diseases. J Neurogastroenterol Motil. 2015;21(2):273-282.
doi pubmed pmc - Mayer EA, Craske M, Naliboff BD. Depression, anxiety, and the gastrointestinal system. J Clin Psychiatry. 2001;62(Suppl 8):28-36, discussion 37.
pubmed - Budavari AI, Olden KW. Psychosocial aspects of functional gastrointestinal disorders. Gastroenterol Clin North Am. 2003;32(2):477-506.
doi pubmed - Haug TT, Mykletun A, Dahl AA. Are anxiety and depression related to gastrointestinal symptoms in the general population? Scand J Gastroenterol. 2002;37(3):294-298.
doi pubmed - Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011;62(6):591-599.
pubmed - Williams M, Budavari A, Olden KW, Jones MP. Psychosocial assessment of functional gastrointestinal disorders in clinical practice. J Clin Gastroenterol. 2005;39(10):847-857.
doi pubmed - Ruan X, Chen J, Sun Y, Zhang Y, Zhao J, Wang X, Li X, et al. Depression and 24 gastrointestinal diseases: a Mendelian randomization study. Transl Psychiatry. 2023;13(1):146.
doi pubmed pmc - Soderquist F, Syk M, Just D, Kurbalija Novicic Z, Rasmusson AJ, Hellstrom PM, Ramklint M, et al. A cross-sectional study of gastrointestinal symptoms, depressive symptoms and trait anxiety in young adults. BMC Psychiatry. 2020;20(1):535.
doi pubmed pmc - Banerjee A, Sarkhel S, Sarkar R, Dhali GK. Anxiety and depression in irritable bowel syndrome. Indian J Psychol Med. 2017;39(6):741-745.
doi pubmed pmc - Bulut Cakmak B, Ozkula G, Isikli S, Ozkan Goncuoglu I, Ocal S, Altinoz AE, Taskintuna N. Anxiety, depression, and anger in functional gastrointestinal disorders: a cross-sectional observational study. Psychiatry Res. 2018;268:368-372.
doi pubmed - Staudacher HM, Black CJ, Teasdale SB, Mikocka-Walus A, Keefer L. Irritable bowel syndrome and mental health comorbidity - approach to multidisciplinary management. Nat Rev Gastroenterol Hepatol. 2023;20(9):582-596.
doi pubmed pmc - Talley NJ, Boyce PM, Jones M. Predictors of health care seeking for irritable bowel syndrome: a population based study. Gut. 1997;41(3):394-398.
doi pubmed pmc - Cantarero-Prieto D, Moreno-Mencia P. The effects of gastrointestinal disturbances on the onset of depression and anxiety. PLoS One. 2022;17(1):e0262712.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.