| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://gr.elmerpub.com |
Original Article
Volume 17, Number 5-6, December 2024, pages 205-211
Evaluating the Impact of Phosphatidylethanol Testing on Hospital Outcomes
Rakahn Haddadina, e, Steven Molinab, George Tradc, John Ryanc, Robert Gishd
aDepartment of Internal Medicine, HCA Healthcare; MountainView Hospital, Las Vegas, NV, USA
bUniversity of California Riverside, School of Medicine, Riverside, CA, USA
cDepartment of Gastroenterology, HCA Healthcare; Southern Hills Hospital and Medical Center, Las Vegas, NV, USA
dHepatitis B Foundation, Doylestown, PA, USA
eCorresponding Author: Rakahn Haddadin, Department of Internal Medicine, HCA Healthcare; MountainView Hospital, Las Vegas, NV 89128, USA
Manuscript submitted October 17, 2024, accepted December 21, 2024, published online December 28, 2024
Short title: Evaluating PEth Testing
doi: https://doi.org/10.14740/gr1790
| Abstract | ▴Top |
Background: Alcohol dependence remains a significant global health issue, exacerbated by the coronavirus disease 2019 (COVID-19) pandemic. Phosphatidylethanol (PEth), a direct biomarker of recent alcohol consumption, offers improved specificity, sensitivity, and a longer detection window of 2 - 4 weeks compared to traditional biomarkers. This study evaluates the association between PEth testing and hospital outcomes in hospitalized patients by comparing outcomes among patients with positive PEth and negative PEth test results.
Methods: This retrospective cohort study used data from the TriNetX database, comprising de- identified medical records from 66 US healthcare organizations from 2015 to 2024. The study population included patients with documented PEth test results. Patients were divided into two groups: positive PEth test results (≥ 20 ng/mL) and negative PEth test results (≤ 19 ng/mL). Propensity score matching was performed to minimize bias, balancing for age, sex, race, ethnicity, and comorbidities such as cirrhosis, diabetes mellitus, hypertension, coronary artery disease, and chronic obstructive pulmonary disease (COPD). Key hospital outcomes assessed included mortality, delirium tremens, endoscopy/colonoscopy, liver transplant status, liver transplant rejection, liver transplant complications, hepatorenal syndrome, intensive care unit (ICU) admission, hepatic encephalopathy, and sarcopenia. These outcomes were chosen based on their prevalence in patients with alcohol use.
Results: Patients with positive PEth results demonstrated significantly worse outcomes compared to patients in the negative PEth group. Positive PEth results were associated with higher mortality (odds ratio, 10.037; P < 0.001), ICU admissions, and rates of complications such as hepatorenal syndrome, hepatic encephalopathy, and sarcopenia. Postoperative liver transplant complications and rejection were also more frequent in the positive cohort.
Conclusions: This study highlights the association between recent alcohol use, as identified by PEth testing, and severe hospital outcomes. While PEth testing provides an objective measure of recent alcohol consumption, further research is needed to explore its role in improving clinical outcomes and guiding interventions for patients with alcohol use.
Keywords: Phosphatidylethanol; PEth testing; Alcohol dependence; Patient outcomes
| Introduction | ▴Top |
Alcohol dependence is an increasing global health problem. Since the coronavirus disease 2019 (COVID-19) pandemic, the USA alone saw roughly 178,000 deaths during 2020 - 2021 from alcohol use, a 29% increase from 2016 to 2017 [1]. Alcohol misuse places a great burden on the healthcare system as it constitutes a major source of morbidity and mortality; more than 28.3 million people in the USA have alcohol use disorder (AUD) [2, 3]. About two-thirds of alcohol-related deaths are from chronic conditions such as heart disease, alcohol-associated liver disease (ALD), and cancer [4].
Some alcohol biomarkers are valuable for uncovering drinking habits. Traditional indirect markers, such as carbohydrate-deficient transferrin (CDT) and γ-glutamyltransferase (GGT), are useful for the identification of prolonged or excessive consumption [5]. Blood alcohol concentration (BAC) or blood and urine ethyl glucuronide (EtG) and ethyl sulfate (EtS) are direct markers, specifically used for the detection of recent alcohol consumption. Direct markers are metabolites of alcohol, making them honest reflections of alcohol consumption, and are often applied in the management of the treatment-seeking AUD population [6].
Alcohol consumption biomarkers have evolved significantly over the past several years. Although not routinely used, EtG testing in hair and fingernails has been studied as a potential long-term alcohol biomarker, with EtG levels in fingernails showing notable promise as a quantitative indicator of alcohol use [7]. An additional promising testing parameter is phosphatidylethanol (PEth), a direct alcohol use biomarker, which has a sensitivity range of 97-100% and a specificity range of 66-96% for detecting alcohol use as reported by the American Association for the Study of Liver Diseases (AASLD) [8]. These findings underscore the utility of PEth as a reliable biomarker for alcohol consumption. BAC, urine EtG, and urine EtS have shorter detection windows, just 2 - 4 days, making PEth testing advantageous over these other testing methods [9-11].
PEth is an abnormal phospholipid synthesized by the enzyme phospholipase D (PLD) in the presence of ethanol within the cell membranes of most animal organs, with 48 identified homologs in the blood [10]. PEth is rapidly broken down in most tissues; however, red blood cells (RBCs) exhibit a unique characteristic that slows its elimination [12]. Unlike other cell types, RBCs lack the activity of certain enzymes, such as phosphatidylcholine phospholipase C (PLC), which likely contributes to their inability to efficiently degrade PEth [12]. This results in an imbalance between PEth formation and degradation within RBCs, causing it to accumulate in their membranes [12]. In other tissues, such as pancreatic islets, hepatocytes, and neutrophils, PEth is cleared more quickly, with a half-life of only 0.5 - 2 h [12]. In contrast, this accumulation in RBCs gives PEth a longer half-life in whole blood, ranging from approximately 4 to 7 days. This extended presence in RBCs makes PEth a reliable biomarker for detecting recent and even chronic alcohol consumption. PEth levels can remain detectable for up to 28 days depending on the consumed amount of ethanol, making this biomarker well-suited for monitoring abstinence, identifying relapse, and evaluating patient drinking behaviors [13].
Homolog 16:0/18:1 is the most commonly used in clinical and forensic investigations, as it accounts for the largest proportion of PEth produced following alcohol consumption [9, 10]. After a single ethanol dose, PEth can be found in the blood of social drinkers and individuals with AUD, reaching detectable levels 30 min to 1 h after alcohol consumption and peaking 90 - 120 min after cessation of drinking [9].
Objective measures of alcohol use are imperative for the effective treatment of AUD and other medical conditions causing morbidity and mortality from long-term alcohol misuse, as self-reports of abstinence and reduced alcohol use are highly subjective to recall bias [14]. Drinking experiments have shown correlations between reported ethanol intake in patients with AUD and blood PEth levels, helping discriminate between social, moderate, and chronic ethanol use, and providing threshold levels considered typical [15].
This study hypothesizes that PEth testing identifies individuals at greater risk for adverse alcohol-related health outcomes.
| Materials and Methods | ▴Top |
Data source
We conducted an analysis using data from the TriNetX database. The TriNetX database is a global federated health research network providing access to electronic medical records across large healthcare organizations. The data were obtained from 66 healthcare organizations across the United States, which included academic and non-academic hospitals. Patients in the database were all hospitalized individuals with PEth testing during 2015 - 2024.
Ethical compliance with human study
The data reviewed are a secondary analysis of existing data, does not involve intervention or interaction with human subjects, and are de-identified per the de-identification standard defined in Section §164.514(a) of the HIPAA Privacy Rule. The process of de-identifying data is attested to through a formal determination by a qualified expert as defined in Section §164.514(b)(1) of the HIPAA Privacy Rule - this formal determination by a qualified expert, refreshed in December 2020.
Study population
TriNetX was queried using the Internal Classification of Diseases 10th version, clinical modification (ICD-10 CM) codes. Inclusion criteria for the patient population were hospitalized patients and PEth test results. Patients who were hospitalized and then obtained a PEth test during hospitalization were included in the study. Table 1 shows patient characteristics for the patients admitted. The analysis compared patients with positive PEth test results to those with negative PEth test results (Fig. 1). The comparison between patients with positive and negative PEth test results was conducted to evaluate alcohol exposure as a whole and its association with clinical outcomes in the patient population. We chose not to limit this analysis to those with fibrosis or cirrhosis to maintain the inclusivity of the entire study cohort and to explore the potential impact of alcohol use across different stages of liver disease. This approach allows for a more comprehensive understanding of alcohol exposure within the study population. There were no exclusion criteria.
 Click to view | Table 1. Patient Characteristics |
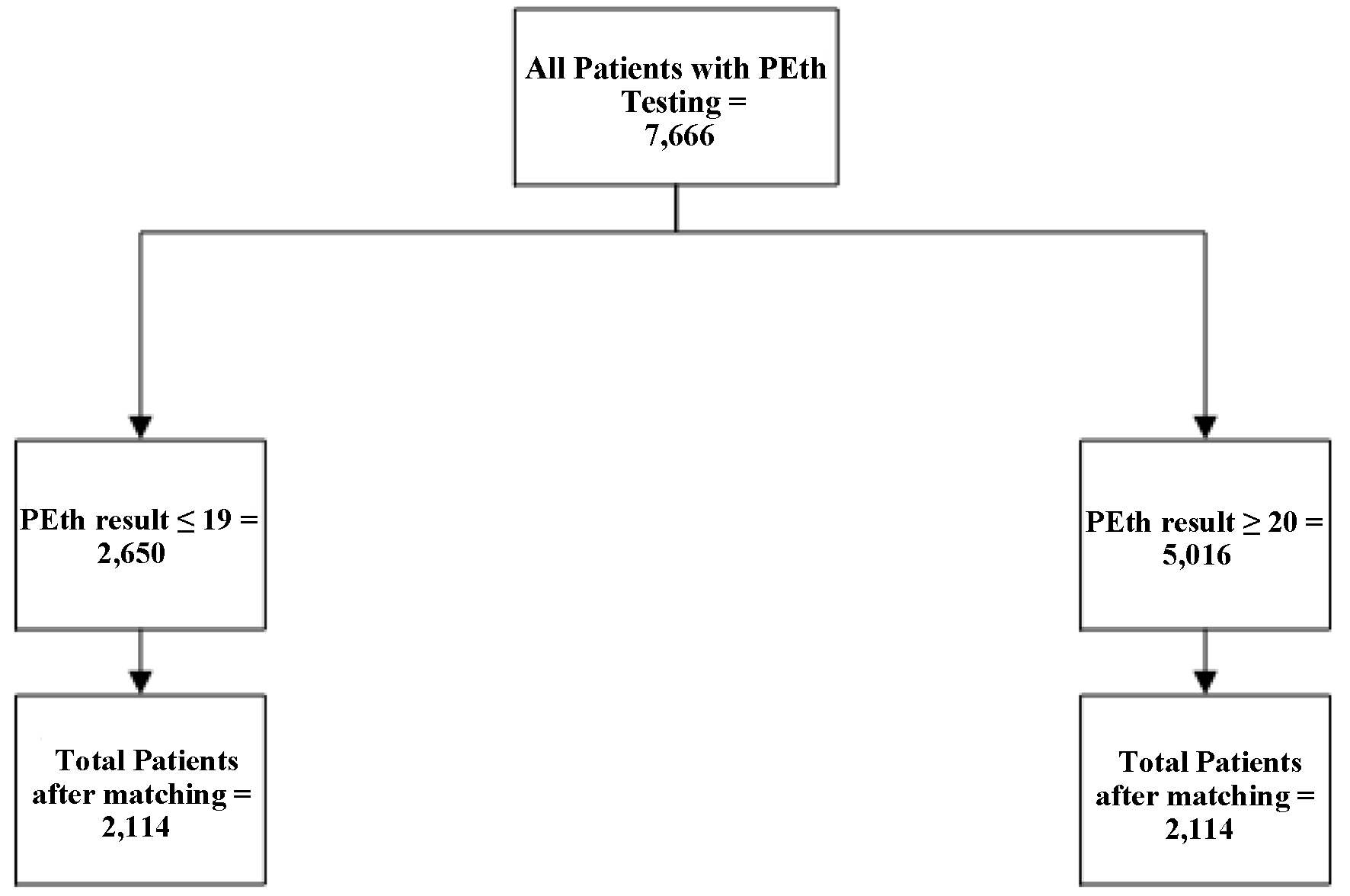 Click for large image | Figure 1. Analysis of patient breakdown. |
High PEth patients vs. low PEth patients
Cohort 1 included 5,016 patients with a PEth test result of 20 ng/mL or higher (i.e., positive PEth test), while cohort 2 included 2,650 patients with a PEth test result of 19 ng/mL or lower (i.e., negative PEth test). All patients in this analysis had undergone PEth testing, totaling 7,666. After matching, each cohort for this analysis had 2,114 patients.
Study outcomes and variables
There were a total of 10 primary outcomes analyzed in this study, selected based on their clinical relevance to the patient population and their importance in reflecting disease progression, complications, or healthcare utilization. These outcomes included mortality, delirium tremens (DT), colonoscopy/endoscopy, liver transplant (LT) listing, LT rejection, LT complications, hepatorenal syndrome (HRS), ICU admission, hepatic encephalopathy (HE), and sarcopenia. The selection was guided by their frequency in the database and their significance in patient outcomes. Notably, the outcomes included both diagnoses and procedures to capture a comprehensive picture of patient morbidity and treatment.
ICD-10 codes, procedure codes, and CPT codes were used to identify these outcomes, with details provided in Supplementary Material 1 (gr.elmerpub.com). All variables were categorized as binary (patients having the condition versus not having the condition). This approach was designed to ensure consistent classification and facilitate meaningful comparisons.
Statistical analysis
To minimize bias and ensure comparability between the cohorts, we employed propensity score matching. This statistical technique was used to create matched pairs of patients from the cohorts based on age, sex, ethnicity, and common comorbidities such as cirrhosis, diabetes mellitus, hypertension, coronary artery disease, chronic obstructive pulmonary disease (COPD), and race. The goal was to create two cohorts that were similar concerning these baseline characteristics, thereby isolating the effect of PEth test results in the two cohorts. Matching was done to reduce bias by ensuring the groups being compared shared similar characteristics. This allowed for better isolation of the effect of the variable of interest.
Following propensity score matching, we conducted several analyses to assess differences between the cohorts. We employed odds ratio (OR) tests to compare the two cohorts. Overall, these methods provided a robust framework for evaluating the effects of PEth test results on related outcomes, ensuring a thorough comparison.
| Results | ▴Top |
High PEth patients vs. low PEth patients
The cohort with PEth levels ≥ 20 ng/mL (n = 2,114) had significantly higher mortality (251 deaths, OR = 10.037). DT was observed in 17 patients in the elevated PEth cohort but not in the lower PEth cohort, preventing analysis due to insufficient cell size. Colonoscopy or endoscopy procedures were more frequent in the elevated PEth cohort (463 vs. 118; OR = 4.744). LT status was more common in the elevated cohort (185 vs. 112; OR = 1.714). LT rejection was higher in the elevated PEth cohort (22 vs. 10; OR = 2.213). LT complications were higher in the elevated cohort (56 vs. 20; OR = 2.849), as was HRS (84 vs. 16; OR = 5.426). ICU admissions were markedly higher in the elevated cohort (318 vs. < 10; OR = 37.235), as was HE (205 vs. 151; OR = 1.396). Sarcopenia was documented in 31 patients in the elevated cohort vs. 10 in the lower cohort (OR = 3.131) (Table 2).
 Click to view | Table 2. Patient Outcomes |
| Discussion | ▴Top |
Our study demonstrated that positive PEth testing (≥ 20 ng/mL), indicative of recent alcohol use, was associated with significantly worse hospital outcomes. Patients in this cohort experienced higher mortality, increased ICU admissions, and greater prevalence of complications such as HRS, HE, and LT rejection compared to those with lower PEth levels. These findings support our hypothesis that recent alcohol consumption, as measured by PEth, correlates with poorer clinical outcomes in hospitalized patients.
Threshold levels considered typical of patients with chronic AUD have been proposed, but absolute cut-offs have yet to be determined [16]. In our study, PEth levels of 20 ng/mL or higher were considered positive PEth test results, while 19 ng/mL or lower were considered negative PEth test results. This study examined the association between positive PEth testing (≥ 20 ng/mL), an objective biomarker of recent alcohol use, and hospital outcomes in patients. These findings highlight the clinical utility of PEth testing for identifying high-risk patients.
Key findings and clinical implications
Positive PEth testing was associated with markedly worse outcomes across multiple measures. Mortality risk was 10-fold higher in the positive cohort compared to the negative cohort (P < 0.001), supporting the link between recent alcohol use, advanced ALD, and increased mortality [14]. AUD is a major contributor to morbidity and mortality, implicated in over 200 ICD-10 conditions [17]. The significantly higher rates of ICU admission (P < 0.0001) and complications such as HE (P = 0.003) and HRS (P < 0.001) in the positive cohort underscore the impact of ongoing alcohol use on disease progression.
DT, a life-threatening complication of alcohol withdrawal, was observed exclusively in the positive PEth cohort, affecting 17 patients. DT, which occurs in 5-10% of alcohol-dependent individuals, carries a mortality rate of 5-15% if untreated [18]. The presence of DT in patients with positive PEth results underscores the ability of PEth testing to objectively identify recent alcohol use, which is a critical risk factor for alcohol withdrawal and its complications. Alcohol withdrawal, particularly severe forms like DT, typically occurs when patients with recent heavy alcohol use suddenly reduce or stop drinking, such as during hospitalization. PEth testing provides an objective and quantifiable measure of recent alcohol consumption, which can help clinicians identify patients at risk for withdrawal syndromes even when self-reported alcohol use is unreliable or underreported.
Unlike self-reported alcohol use, PEth testing is not subject to recall or social desirability biases, making it a more reliable tool for identifying patients with AUD who may be at heightened risk for adverse hospital outcomes like DT. By proactively identifying these patients, clinicians can initiate appropriate monitoring and preventive interventions, such as early pharmacologic treatment for alcohol withdrawal, reducing the risk of DT and other severe complications.
The positive PEth cohort also required significantly more endoscopic procedures (P < 0.001), reflecting a higher prevalence of alcohol-related gastrointestinal conditions. Esophageal and colorectal cancers, which rank among the most common and deadliest gastrointestinal cancers globally, are closely linked to alcohol use [19]. Incorporating PEth testing into routine screening protocols could improve early detection and management of such complications.
In the context of liver transplantation, patients with positive PEth results were more likely to be listed for transplant (P < 0.001), reflecting more advanced disease. LT rejection was also significantly more frequent in this group (P = 0.033), consistent with studies showing that chronic rejection remains a major cause of graft failure despite advancements in immunosuppressive regimens [20]. Postoperative LT complications, including biliary tract issues, were nearly three times higher in the positive PEth cohort (P < 0.001), reflecting the worse outcomes observed in patients with recent alcohol use. This finding highlights the association between positive PEth results and ongoing alcohol use or advanced liver disease, which are well-known contributors to post-transplant complications.
Importantly, the measurement of PEth itself does not cause or reduce complications; rather, it identifies a subgroup of patients at higher risk due to their recent alcohol use. PEth testing serves as a valuable tool for objectively identifying these patients, enabling closer monitoring and tailored interventions to potentially mitigate post-transplant risks and improve outcomes over time [13].
Sarcopenia, a condition linked to malnutrition and alcohol-related muscle protein depletion, was also significantly more prevalent in the positive PEth cohort (P = 0.001). The association between alcohol use and sarcopenia underscores the need for nutritional interventions and physical rehabilitation in at-risk patients.
Addressing biases and study limitations
Several limitations and potential biases must be considered. The cross-sectional design precludes establishing causality or temporality between PEth levels and hospital outcomes. The timing of PEth testing relative to clinical events remains unclear, raising the possibility of reverse causation. For example, the “sick quitter” phenomenon, where patients with advanced liver disease reduce alcohol consumption, could result in negative PEth tests despite prior heavy alcohol use. This phenomenon may lead to underestimation of the true impact of alcohol on disease outcomes. Selection bias is another significant concern. Patients undergoing PEth testing were likely those with known or suspected AUD or ALD, inherently predisposing this group to worse outcomes.
The use of a PEth threshold of ≥ 20 ng/mL, while indicative of any recent alcohol consumption, does not account for varying levels of alcohol use. Exploring higher thresholds could provide a more nuanced understanding of the dose-response relationship between alcohol use and clinical outcomes. Additionally, the study did not include self-reported alcohol use, which remains a practical tool in clinical settings despite its susceptibility to recall and social desirability biases. Future studies should compare self-reported data with PEth results to evaluate the biomarker’s added value.
Strengths and future directions
This study’s strengths include the use of PEth, a reliable biomarker for recent alcohol use, and the large sample size, which enabled detailed subgroup analyses. However, prospective studies are needed to address the limitations of this study. Longitudinal designs could clarify the temporal relationship between PEth levels and clinical outcomes, helping to disentangle the effects of alcohol use from disease progression. Exploring the predictive value of PEth testing for outcomes such as ICU admission, mortality, and transplant rejection would further validate its clinical utility.
Additionally, future research should investigate the integration of PEth testing into routine clinical workflows. This includes evaluating its cost-effectiveness, feasibility, and impact on patient outcomes. For example, PEth testing could be used to guide transplant eligibility decisions, monitor abstinence, and identify patients at risk for alcohol-related complications.
Conclusions
Positive PEth testing, another direct biomarker of recent alcohol use, is strongly associated with worse hospital outcomes, including higher mortality, increased ICU admissions, and greater prevalence of complications such as HE, HRS, and LT rejection. These associations are driven by ongoing alcohol use, not by PEth testing itself. PEth serves as an objective tool to identify patients with recent alcohol consumption, enabling clinicians to recognize high-risk individuals who may benefit from targeted interventions and closer monitoring. However, the study’s limitations, including selection bias, lack of temporality, and absence of self-reported alcohol use data, must be considered. Further research, particularly prospective studies, is necessary to validate these findings and to refine the role of PEth testing in improving the care and outcomes of patients with AUD.
| Supplementary Material | ▴Top |
Suppl 1. ICD-10 codes, procedure codes, and CPT codes.
Acknowledgments
We thank Kelly Schrank, MA, ELS, of Bookworm Editing Services LLC for her editorial services in preparing the manuscript for publication.
Financial Disclosure
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA author(s) and does not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Conflict of Interest
Robert G. Gish: owns stock in Abacus, AngioCrine, JBS Science, and Virion. He is on the speakers’ bureau for AstraZeneca, BMS, Diasorin, Eisai, Ipsen Biopharmaceuticals, Mallinckrodt, and VBI Vaccines. He has other interests in Arrowhead, CymaBay Therapeutics, Durect, Kezar Life Sciences, Sagimet, and Takeda. He consults for Fibronostics, Fujifilm/Wako, Perspectum, Quest, Sonic Incytes, Abacus, Abbott, Albireo, Aligos, Altimunne, Antios, Arrowhead, AstraZeneca, Audentes Therapeutics, Corcept, Dynavax, Effectus, Eisai, Enyo, Genlantis, Gerson Lehrman Group, GlaxoSmithKline, Helios, Ipsen, Janssen, JBS Science, Kinnate Bio, Merck, Precision BioSciences, Pfizer, Seres Therapeutics, Topography Health, Tune Therapeutics, Venatorx, and Virion. He advises Dynavax, Enyo, Helios, Janssen, Merck, Pfizer, and Prodigy. He owns stock in, consults for, and advises HepQuant. He is on the speakers’ bureau, consults for and advises AbbVie. He is on the speakers’ bureau, consults for, advises, and received grants from Gilead Sciences Inc. He owns stock in, consults for, and advises HepaTX. He owns stock in and consults for Eiger. He owns stock in, consults for, and advises Genlantis. He is on the speakers’ bureau, consults for, and advises Intercept. He is on the speakers’ bureau, consults for, and advises Genentech. The remaining authors have no conflicts to report.
Informed Consent
This retrospective study is exempt from informed consent.
Author Contributions
Conceptualization: RH, SM, and GT; methodology: RH, SM, and GT; writing - original draft preparation: RH, SM, and GT; writing - review and editing: RH, SM, and GT; visualization: RH, SM, and GT; supervision: JR and RG. All authors have read and agreed to the published version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article and its supplementary information file.
| References | ▴Top |
- Esser MB, Sherk A, Liu Y, Naimi TS. Deaths from excessive alcohol use - United States, 2016-2021. MMWR Morb Mortal Wkly Rep. 2024;73(8):154-161.
doi pubmed - Substance Abuse and Mental Health Services Administration. 2023 National Survey on Drug Use and Health (NSDUH) Releases. Published 2023. Accessed October 14, 2024.
- Substance Abuse and Mental Health Services Administration. 2023 NSDUH Detailed Tables. Published 2023. Accessed October 14, 2024. https://www.samhsa.gov/data/report/2023-nsduh-detailed-tables.
- Centers for Disease Control and Prevention. Alcohol-related disease impact application. Accessed March 21, 2024. www.cdc.gov/ardi.
- Schrock A, Thierauf-Emberger A, Schurch S, Weinmann W. Phosphatidylethanol (PEth) detected in blood for 3 to 12 days after single consumption of alcohol-a drinking study with 16 volunteers. Int J Legal Med. 2017;131(1):153-160.
doi pubmed - Gruner Nielsen D, Andersen K, Sogaard Nielsen A, Juhl C, Mellentin A. Consistency between self-reported alcohol consumption and biological markers among patients with alcohol use disorder - A systematic review. Neurosci Biobehav Rev. 2021;124:370-385.
doi pubmed - Berger L, Fendrich M, Jones J, Fuhrmann D, Plate C, Lewis D. Ethyl glucuronide in hair and fingernails as a long-term alcohol biomarker. Addiction. 2014;109(3):425-431.
doi pubmed - Crabb DW, Im GY, Szabo G, Mellinger JL, Lucey MR. Diagnosis and treatment of alcohol-associated liver diseases: 2019 practice guidance from the American Association for the study of liver diseases. Hepatology. 2020;71(1):306-333.
doi pubmed - Andresen-Streichert H, Muller A, Glahn A, Skopp G, Sterneck M. Alcohol biomarkers in clinical and forensic contexts. Dtsch Arztebl Int. 2018;115(18):309-315.
doi pubmed - Helander A, Hermansson U, Beck O. Dose-response characteristics of the alcohol biomarker phosphatidylethanol (PEth)-a study of outpatients in treatment for reduced drinking. Alcohol Alcohol. 2019;54(6):567-573.
doi pubmed - Lopez-Cruzan M, Roache JD, Hill-Kapturczak N, Karns-Wright TE, Dougherty DM, Sanchez JJ, Koek W, et al. Pharmacokinetics of phosphatidylethanol 16:0/20:4 in human blood after alcohol intake. Alcohol Clin Exp Res. 2018;42(11):2094-2099.
doi pubmed - Javors MA, Hill-Kapturczak N, Roache JD, Karns-Wright TE, Dougherty DM. Characterization of the pharmacokinetics of phosphatidylethanol 16:0/18:1 and 16:0/18:2 in human whole blood after alcohol consumption in a clinical laboratory study. Alcohol Clin Exp Res. 2016;40(6):1228-1234.
doi pubmed - Fleming MF, Smith MJ, Oslakovic E, Lucey MR, Vue JX, Al-Saden P, Levitsky J. Phosphatidylethanol detects moderate-to-heavy alcohol use in liver transplant recipients. Alcohol Clin Exp Res. 2017;41(4):857-862.
doi pubmed - Lohoff FW. Targeting unmet clinical needs in the treatment of alcohol use disorder. Front Psychiatry. 2022;13:767506.
doi pubmed - Perilli M, Toselli F, Franceschetto L, Cinquetti A, Ceretta A, Cecchetto G, Viel G. Phosphatidylethanol (PEth) in blood as a marker of unhealthy alcohol use: a systematic review with novel molecular insights. Int J Mol Sci. 2023;24(15):12175.
doi pubmed - Hahn JA, Fatch R, Barnett NP, Marcus GM. Phosphatidylethanol vs transdermal alcohol monitoring for detecting alcohol consumption among adults. JAMA Netw Open. 2023;6(9):e2333182.
doi pubmed - Rehm J, Shield KD. Global burden of alcohol use disorders and alcohol liver disease. Biomedicines. 2019;7(4):99.
doi pubmed - Rahman A, Paul M. Delirium Tremens. In: StatPearls. Treasure Island (FL). 2024.
pubmed - Jardim SR, de Souza LMP, de Souza HSP. The rise of gastrointestinal cancers as a global phenomenon: unhealthy behavior or progress? Int J Environ Res Public Health. 2023;20(4):3640.
doi pubmed - Angelico R, Sensi B, Manzia TM, Tisone G, Grassi G, Signorello A, Milana M, et al. Chronic rejection after liver transplantation: Opening the Pandora's box. World J Gastroenterol. 2021;27(45):7771-7783.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.