| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://gr.elmerpub.com |
Short Communication
Volume 18, Number 3, June 2025, pages 149-151
The Reverse Red-Green-Blue Rule: A Color-Coded Approach for Simplified Achalasia Diagnosis via High-Resolution Manometry
Mohammed Abdulrasaka, b, d, Sohail Hootaka, b, Mostafa Mohragc, Ali M. Someilic
aDepartment of Clinical Sciences, Lund University, 22100 Malmo, Sweden
bDepartment of Gastroenterology and Nutrition, Skane University Hospital, 21428 Malmo, Sweden
cDepartment of Medicine, Faculty of Medicine, Jazan University, Jazan 45142, Saudi Arabia
dCorresponding Author: Mohammed Abdulrasak, Department of Clinical Sciences, Lund University, 22100 Malmo, Sweden
Manuscript submitted March 26, 2025, accepted May 15, 2025, published online June 4, 2025
Short title: Color-Based HRM Interpretation
doi: https://doi.org/10.14740/gr2040
| Abstract | ▴Top |
Background: Achalasia is a rare motility disorder of the esophagus. The diagnosis involves clinical suspicion based on history details and results of high-resolution manometry (HRM) as recommended by the Chicago classification (CCv4.0). Interpreting data obtained through HRM can be complex especially for the novice user.
Methods: We propose therefore a color-based algorithm involving the “reversed red-green-blue (RGB)” rule as a simplified way to establish the diagnosis based on colors obtained through the HRM pressure sensors. The rule is based on the simple acknowledgment of the dominant color present in the mid-portion of the HRM figure such that, for type I (classic) achalasia, the blue color illustrates the minimal pressurization and absent peristalsis. In type II (pan-pressurized) achalasia, the green color illustrates pan-esophageal pressurization, while in type III (spastic) achalasia, red color illustrates the spastic contractions.
Results: This rule, which we present as a conceptual framework and has not yet been prospectively validated, provides an intuitive tool for clinicians dealing with HRMs diagnosing achalasia.
Conclusion: Further studies are required to assess the diagnostic accuracy of this rule, alongside the potential for incorporating such rules into artificial intelligence (AI)-based models for manometric diagnosis of esophageal motility disorders.
Keywords: Achalasia; High-resolution manometry; Memory aid
| Introduction | ▴Top |
Achalasia is a rare esophageal motility disorder characterized by loss of lower esophageal sphincter (LES) relaxation and afterwards loss of peristalsis in the distal esophagus [1]. This is theorized to be related to degeneration of neuronal control through loss of ganglion cells in the esophageal wall [2]. It is unclear what the trigger for this condition is; however, several theories revolve around it occurring as a post-viral phenomenon related to herpes simplex virus (HSV) [3], varicella-zoster virus (VZV) [4], and other viral infections [5]. The exact trigger is however still not exactly elucidated [6].
The diagnosis is based on the high-resolution manometry (HRM) data as per the Chicago classification version 4.0 (CCv4.0) [7]. This remains the gold standard for diagnosing achalasia with its subtypes, yet the difficulty lies in the multitude of values that are required to establish the diagnosis which makes it difficult for non-experts to interpret these values. These values include integrated relaxation pressure (IRP), distal latency (DL), and distal contractile integral (DCI) [8].
The HRM plots already use color gradients to visualize patterns obtained regarding esophageal pressure patterns such that the blue color indicates minimal pressure, green color indicates moderate pressure, and red color indicates high pressure generated [9]. In spite of this, and to the best of our knowledge, we are unaware of any standardized rule for rapid achalasia identification based on the already represented HRM color-coded plots. We hope that the reverse red-green-blue (RGB) rule, blue-green-red rule, which is directly associated with colors obtained through HRM plots, would aid clinicians in easily recognizing achalasia. In addition, we hope that this rule will be implemented in artificial intelligence (AI)-assisted software to help expedite esophageal motility disorder diagnostics.
| Methods | ▴Top |
The primary colors, described through the mnemonic RGB, constitute the basis for all the colors generated when mixed together, with the red color being at the longest wavelength, green in the middle, and blue the shortest wavelength of the three [10]. These colors constitute the basis for the plots obtained from HRM software, signifying a continuum from low pressure (blue color) to “mid-pressure” (green) to high pressure (red). Type I achalasia involves the absence of peristalsis with minimal pressurization, type II achalasia involves pan-esophageal pressurization, while type III achalasia involves the presence of premature contractions with abnormal, spastic peristaltic waves [11]. The Chicago classification relies heavily on numerical values, mainly the IRP, DL, and DCI [7]. These are, however, quite tedious and therefore HRM interpretation has a steep learning curve for early-level trainees [12]. Figure 1 illustrates the typical HRM pattern of each achalasia subtype alongside the association with the earlier mentioned “reverse RGB” rule.
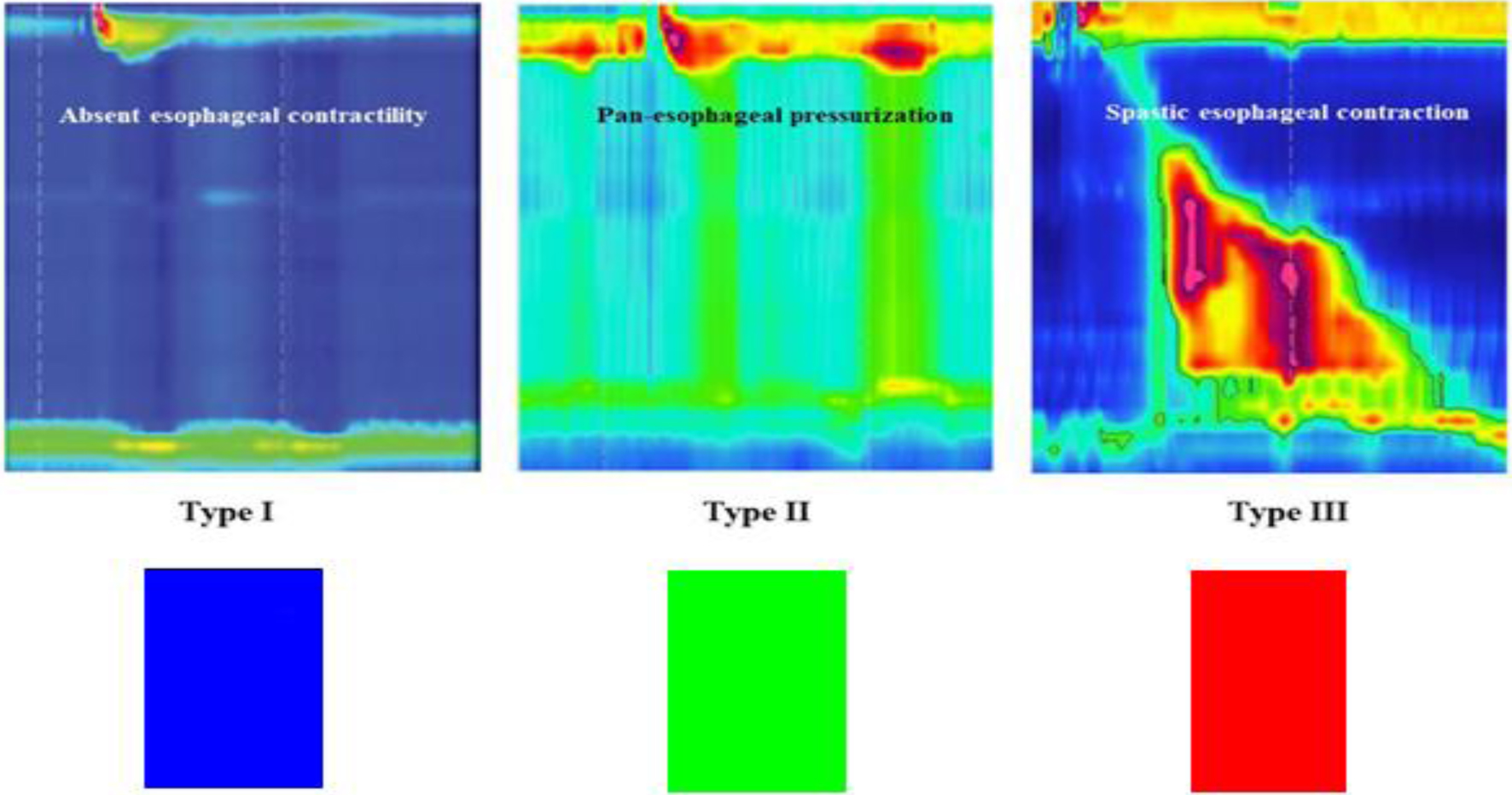 Click for large image | Figure 1. The association of the HRM plots with the “reverse RGB”. The “reverse RGB” is named so because it starts from blue (type I) to green (type II) to red (type III) which are the dominant colors in each figure. Figure adapted from Reference [1]. Licensed under Creative Commons Attribution 4.0 International License (CC BY 4.0). HRM: high-resolution manometry; RGB: red-green-blue. |
| Results and Discussion | ▴Top |
We believe that this rule, albeit appearing simplistic, is an effective rule especially given it already matching the main colors represented in HRMs when diagnosing each achalasia subtype as illustrated in Figure 1. Such visual aids reduce the cognitive load associated with diagnostic processes in medicine, which is especially relevant in entry-level trainees [13]. In addition, the rule may aid in serving as a simplified framework for these trainees and enhance education in this area, especially given the generally poor competency associated with this specific portion of gastroenterology [14]. Furthermore, the potential for automated pattern recognition of data obtained from HRMs through AI-assisted software is immense, with the possibility of faster and more accurate diagnosis on the basis of such pattern recognition regardless of the numerical data obtained through HRMs [15]. This rule is, for the aforementioned reasons, not intended to replace formal diagnostic algorithms like the Chicago classification, but rather to assist in pattern recognition especially for early trainees. We recognize that certain atypical or overlapping motility patterns may fall outside this simplified model.
In spite of this, there are certain potential limitations to the proposed color-based quick guide. The main one is the lack of validation, as this is necessary to ensure that the color-based approach conforms well to the HRM data as per the Chicago classification. In addition, there needs to be multicenter trials to ensure the sensitivity and specificity of this color-based rule for HRM interpretation, alongside inter-observer reliability. Furthermore, cross-platform validation is necessary given the slight differences present in the visual representation provided by the different manufacturers. To add more, the potential application across other diagnoses within the esophageal motility sphere needs consideration.
Conclusion
The Reverse Red-Green-Blue (RGB) Rule offers a simplified visual classification system for achalasia subtypes, aligning with the characteristic color patterns seen in HRM plots for these diagnoses. This system may improve clinical decision-making, trainee education with regards to HRM interpretation, and potentially AI-based diagnosis. Further validation with multicenter HRM datasets is needed to confirm the rule’s accuracy and clinical adoption, alongside potential for automated HRM diagnosis. We hope that this framework may serve as the basis for further educational tools or automated diagnostic algorithms in the future.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Study conception and design: Mohammed Abdulrasak. Analysis and interpretation of results and draft manuscript preparation: Mohammed Abdulrasak, Mostafa Mohrag, Ali M. Someili, and Sohail Hootak. All authors reviewed the results and approved the final version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Mari A, Abu Baker F, Pellicano R, Khoury T. Diagnosis and management of achalasia: updates of the last two years. J Clin Med. 2021;10(16):3607.
doi pubmed - Ghoshal UC, Daschakraborty SB, Singh R. Pathogenesis of achalasia cardia. World J Gastroenterol. 2012;18(24):3050-3057.
doi pubmed - Castagliuolo I, Brun P, Costantini M, Rizzetto C, Palu G, Costantino M, Baldan N, et al. Esophageal achalasia: is the herpes simplex virus really innocent? J Gastrointest Surg. 2004;8(1):24-30; discussion 30.
doi pubmed - Naik RD, Vaezi MF, Gershon AA, Higginbotham T, Chen JJ, Flores E, Holzman M, et al. Association of achalasia with active varicella zoster virus infection of the esophagus. Gastroenterology. 2021;161(2):719-721.e712.
doi pubmed - Moradi A, Fazlollahi N, Eshraghi A, Gholipour M, Khoshnia M, Javid N, Montazeri SA, et al. Is there any evidence for a viral cause in achalasia? Middle East J Dig Dis. 2018;10(3):169-173.
doi pubmed - Mari A, Khoury T, Sweis R. Achalasia: beyond the basics. Frontline Gastroenterology. 2025;16:59-71.
doi - Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, Babaei A, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil. 2021;33(1):e14058.
doi pubmed - Yadlapati R. High-resolution esophageal manometry: interpretation in clinical practice. Curr Opin Gastroenterol. 2017;33(4):301-309.
doi pubmed - Nigam GB, Vasant DH, Dhar A. Curriculum review : investigation and management of dysphagia. Frontline Gastroenterol. 2022;13(3):254-261.
doi pubmed - Tedore C, Johnsen S. Using RGB displays to portray color realistic imagery to animal eyes. Curr Zool. 2017;63(1):27-34.
doi pubmed - Kahrilas PJ, Boeckxstaens G. The spectrum of achalasia: lessons from studies of pathophysiology and high-resolution manometry. Gastroenterology. 2013;145(5):954-965.
doi pubmed - Gaddam S, Reddy CA, Munigala S, Patel A, Kanuri N, Almaskeen S, Rude MK, et al. The learning curve for interpretation of oesophageal high-resolution manometry: a prospective interventional cohort study. Aliment Pharmacol Ther. 2017;45(2):291-299.
doi pubmed - Young JQ, Van Merrienboer J, Durning S, Ten Cate O. Cognitive Load Theory: implications for medical education: AMEE Guide No. 86. Med Teach. 2014;36(5):371-384.
doi pubmed - DeLay K, Pandolfino JE, Gyawali CP, Frye J, Kaizer A, Menard-Katcher P, Sloan JA, et al. Esophageal manometry competency program improves gastroenterology fellow performance in motility interpretation. Am J Gastroenterol. 2020;115(9):1453-1459.
doi pubmed - Fass O, Rogers BD, Gyawali CP. Artificial intelligence tools for improving manometric diagnosis of esophageal dysmotility. Curr Gastroenterol Rep. 2024;26(4):115-123.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.