| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://gr.elmerpub.com |
Original Article
Volume 18, Number 6, December 2025, pages 308-321
Global Prevalence of Irritable Bowel Syndrome: An Updated Systematic Review and Meta-Analysis
Jhosmer Ballena-Caicedoa, Lupita Ana Maria Valladolid-Sandovala, Fiorella E. Zuzunaga-Montoyaa, Victor Juan Vera-Poncea, b
aFacultad de Medicina (FAMED), Universidad Nacional Toribio Rodriguez de Mendoza de Amazonas (UNTRM), Amazonas, Peru
bCorresponding Author: Victor Juan Vera-Ponce, Facultad de Medicina (FAMED), Universidad Nacional Toribio Rodriguez de Mendoza de Amazonas (UNTRM), Amazonas, Peru
Manuscript submitted October 7, 2025, accepted December 8, 2025, published online December 20, 2025
Short title: Global Prevalence of IBS
doi: https://doi.org/10.14740/gr2095
| Abstract | ▴Top |
Background: Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by abdominal pain and alterations in bowel habits. Previous studies show variability in its prevalence according to region and diagnostic criteria used. The objective was to conduct a systematic review and meta-analysis of the global prevalence of IBS, considering studies that used Rome III and IV criteria.
Methods: A systematic search was conducted in Scopus, Embase, PubMed, Web of Science, and Scielo through March 2024. Observational studies reporting IBS prevalence using Rome III or IV criteria were included. Studies in specific populations, conference abstracts, and gray literature were excluded. Methodological quality was assessed using Munn’s tool for prevalence studies. Meta-analyses were performed using random-effects models with Freeman-Tukey double arcsine transformation, subgroup analyses by probabilistic sampling, meta-regressions by year, and publication bias assessment through funnel plots.
Results: Forty-three studies (26 Rome III, 17 Rome IV) with 188,885 participants were included. The global prevalence was 13.21% (95% confidence interval (CI): 10.70-15.94%) with Rome III and 17.14% (95% CI: 12.00-22.99%) with Rome IV. When considering only studies with probabilistic sampling, prevalences adjusted to 11.19% and 13.28%, respectively. Higher prevalence was found in women (Rome III: 15.69% vs. 11.10% in men; Rome IV: 20.17% vs. 11.45%). Meta-regression showed a trend toward increased prevalence in recent years.
Conclusion: Rome IV showed a higher prevalence than Rome III, possibly due to a more precise definition of abdominal pain. The heterogeneity found suggests the need to standardize methodologies and conduct more studies with probabilistic sampling, especially in underrepresented regions.
Keywords: Irritable bowel syndrome; Abdominal pain; Functional bowel disorders; Prevalence; Meta-analysis; Systematic review
| Introduction | ▴Top |
Irritable bowel syndrome (IBS) has established itself as one of the most common functional gastrointestinal disorders worldwide, characterized by chronic or recurrent abdominal pain associated with alterations in bowel habits in the absence of structural abnormalities [1, 2]. Its complex pathophysiology involves visceral hypersensitivity factors, microbiota dysbiosis, alterations in the gut-brain axis, and psychosocial factors [3]. The diagnosis is established based on the Rome criteria (currently Rome IV), which, throughout its evolution, has allowed greater homogeneity in clinical classification and epidemiological research [4].
Globally, variable IBS prevalence rates have been reported depending on geographical region, study methodology, and, crucially, the version of diagnostic criteria used. A significant meta-analysis published by Oka et al in 2020, which included 53 studies using Rome III criteria, estimated a pooled prevalence of 9.2% (95% confidence interval (CI): 7.6-10.8%) in 395,385 participants from 38 countries [5]. In contrast, in the same work, the pooled prevalence from six studies that applied Rome IV criteria in 82,476 individuals from 34 countries decreased to 3.8% [5]. These marked differences demonstrate the impact of updated diagnostic criteria and reinforce the need for recent studies that unify the findings.
Since the previous publication, new studies have emerged incorporating populations from regions that were previously not included or had limited representation. Additionally, more recent multicenter studies point to the influence of cultural, dietary, and socioeconomic factors on the clinical presentation and frequency of IBS [6, 7]. This geographical expansion of knowledge underscores the importance of updating epidemiological information to recognize emerging patterns and delineate more precise transcontinental comparisons.
In this context, the present study aimed to conduct a systematic review (SR) with a meta-analysis of IBS prevalence worldwide, incorporating new studies published after 2020 [5] and critically considering the application of different diagnostic criteria. Our objective was to provide an updated overview of the global burden of this disorder while exploring the epidemiological and methodological factors that influence its estimates. The results presented here will serve as a foundation for future research directions and for designing clinical interventions and health policies to improve the quality of life of those suffering from IBS.
| Materials and Methods | ▴Top |
Study design
This study was conducted as an SR and meta-analysis of the global prevalence of IBS. Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [8], a specific adaptation for prevalence reviews was used, which allows standardization of the search, selection, and synthesis of studies.
Search strategy
The search followed the Cochrane Collaboration’s methodological recommendations regarding database selection and search strategy development. The following sources were consulted: SCOPUS, Web of Science (including SciELO catalog), PubMed, and EMBASE, due to their broad coverage of biomedical literature. The search was conducted through March 1, 2025. To identify the maximum number of relevant studies on global IBS prevalence, terms related to “irritable bowel syndrome,” “IBS,” “spastic colon,” “irritable colon,” “Rome III,” “Rome IV,” among others, were used, combined through Boolean operators (AND, OR). In each database, descriptors and synonyms were adapted to the corresponding controlled vocabulary (e.g., MeSH in PubMed and Emtree in EMBASE). The detailed search strategy, including terms, synonyms, and applied filters, is described in Supplementary Material 1 (gr.elmerpub.com).
Selection criteria
Observational studies reporting IBS prevalence were included, whether as their primary or secondary objective. Furthermore, only studies that used the Rome III [9] or Rome IV [4] criteria as a diagnostic basis were included. Studies with probabilistic and non-probabilistic sampling were eligible, with no language restrictions on publication. In all cases, a clear presentation of the total sample size and the number (or proportion) of individuals diagnosed with IBS was required.
Studies evaluating populations with specific characteristics (e.g., patients with another defined comorbid disease or exclusively belonging to a particular group), case reports, congress abstracts, letters to the editor, SRs, bibliometric reviews, and conference communications or proceedings books that did not present complete data for prevalence calculation were excluded. Additionally, studies that did not specify the diagnostic criteria used or did not provide sufficient information to calculate prevalence were excluded.
Study selection process
After applying the search strategy across databases, results were exported to Rayyan software for review and screening. Three reviewers (VJVP, JJBC, and LAMVS) searched and selected articles simultaneously and independently, maintaining the blinding function offered by Rayyan. Once this initial phase was completed, the blinding was removed, and each reviewer’s list of articles was compared. In cases of discrepancy, reviewers deliberated until reaching a consensus; if this was not possible, a fourth author (FEZM) intervened to make the final decision regarding study inclusion or exclusion.
Data extraction and qualitative analysis
Articles meeting inclusion criteria were compiled in a Microsoft Excel 2023 template, where data from each study were systematically recorded. Extracted information included: author(s) and publication year, participating Latin American country(ies), study design and data collection period, sample size and demographic characteristics (age, sex), sampling method used, and diagnostic criteria employed for IBS definition. To conduct a comprehensive qualitative analysis, the main conclusions and limitations of the studies were also reviewed, along with relevant epidemiological and clinical context.
Risk of bias assessment
Three reviewers (VJVP, JJBC, and LAMVS) independently conducted risk of bias assessments for all studies included in this review. The tool proposed by Munn et al [9] for prevalence studies was employed due to its relevance in evaluating the methodological quality of this type of research and its wide recognition in the field of SRs.
This instrument considers 10 essential criteria in conducting prevalence studies, such as sample representativeness about the target population, quality of the sampling frame, participant selection method (random or non-random), minimization of non-response bias, direct information collection from subjects, clear and acceptable case definition, reliability and validity of the instrument used, consistency in data collection methods, appropriateness of the prevalence period considered, and adequacy of the denominator used.
Each criterion was assigned a rating of “low risk” (7 - 10 points), “medium risk” (4 - 6 points), or “unclear” (0 - 3 points). If there were discrepancies between the two reviewers, a discussion was held to reach a consensus; if differences persisted, a third researcher’s opinion was sought for the final decision.
Statistical analysis
Quantitative analyses were conducted using R statistical software version 4.2.2. All statistical analyses were performed independently and in duplicate by two investigators (VJVP and JJBC). Results were compared to verify concordance, with special attention to assessments of heterogeneity (I2 statistics and prediction intervals). Disagreements were discussed and resolved by consensus between the two analysts. For the meta-analysis, only studies reporting sufficient data on IBS prevalence were considered, including figures for total participants (n) and number of cases (r).
The metaprop function from the meta package was employed with Freeman-Tukey proportion transformation (sm = “PFT”). This transformation is used to stabilize variance when analyzing prevalence data. CIs were estimated using the Clopper-Pearson method (method.ci = “CP”), which provides exact intervals for proportions. Considering the expected heterogeneity among studies, due to differences in population, diagnostic methods, or design, a random-effects model was applied using the DerSimonian and Laird method (method.tau = “DL”), and standard errors were corrected using the Hartung-Knapp approximation (hakn = TRUE). For subgroup analyses, studies were classified as “probabilistic sampling” when explicit random selection procedures from a defined sampling frame were reported. Studies that did not clearly describe such methods, or that employed convenience, voluntary, or other non-random recruitment strategies, were conservatively classified as “non-probabilistic sampling.”
Heterogeneity was assessed using the I2 statistic and Cochran’s Q test, which are automatically calculated by the metaprop function. Meta-analysis results are summarized in forest plots also generated with the meta package.
Additionally, meta-regressions were performed to investigate the potential influence of continuous variables on IBS prevalence. Specifically, the effect of publication year and diagnostic criteria used (Rome III vs. Rome IV) was evaluated. For this purpose, the rma function from the metafor package in R was used, fitting mixed-effects models where study weights were inversely proportional to variance. Results from these meta-regressions were illustrated through bubble plots, where the size of each bubble corresponds to the statistical weight of the study in the analysis.
| Results | ▴Top |
Article selection
The study selection process was conducted following PRISMA guidelines. The initial search in electronic databases identified 9,046 records, distributed as follows: Scopus (3,801), Embase (1,717), PubMed (1,750), Web of Science (1,709), and Scielo (69). After removing duplicates, 4,464 unique records remained for review. During the screening phase, 4,355 studies were excluded, leaving 109 articles for full-text evaluation. Of these, 59 additional articles were excluded. Finally, 43 studies were selected for qualitative and quantitative synthesis, of which 26 employed Rome III criteria and 17 used Rome IV criteria [10-52] (Fig. 1).
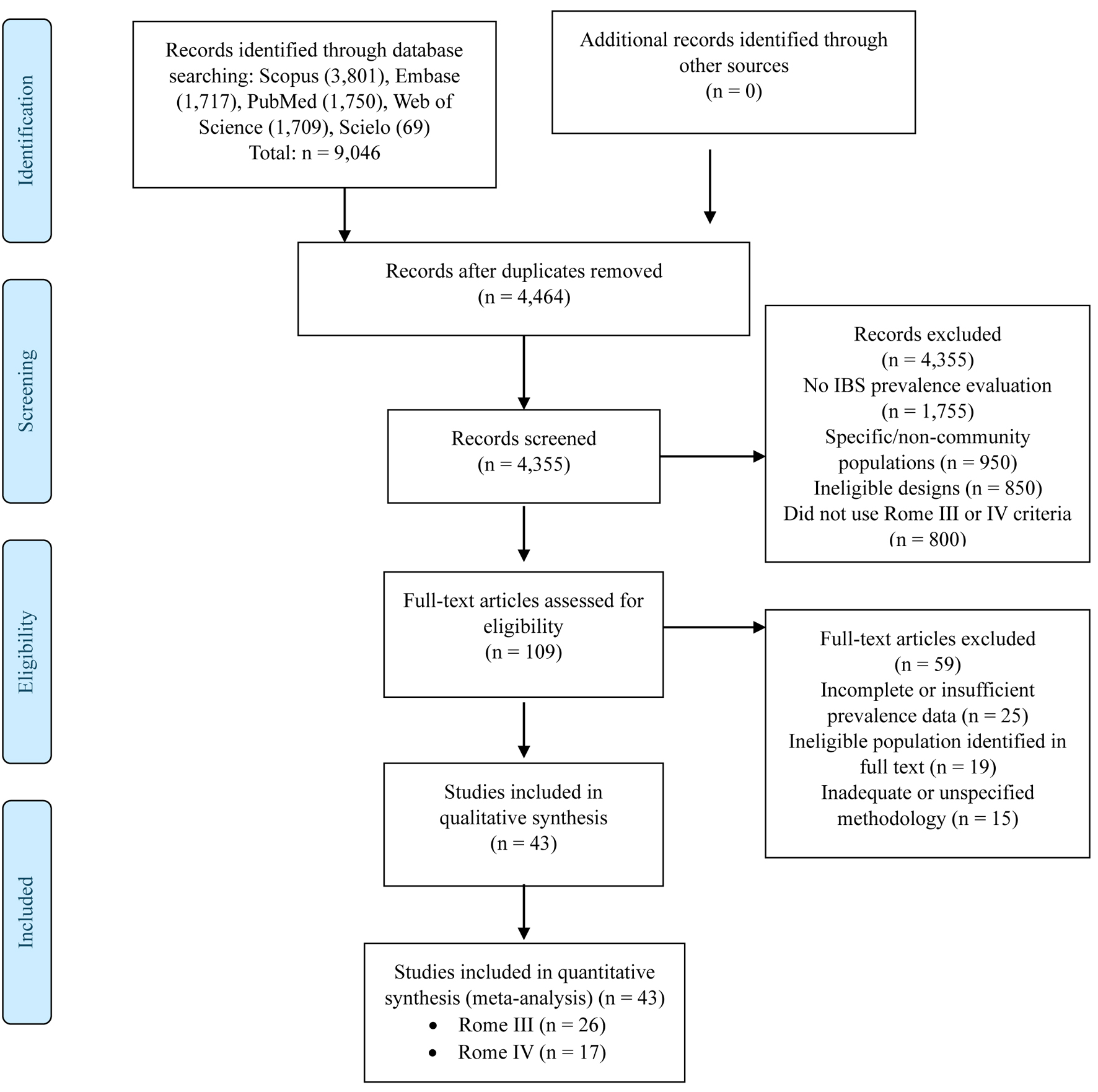 Click for large image | Figure 1. Flowchart of study selection. |
Main characteristics
Forty-three studies published between 2008 and 2024 were included, encompassing a total of 188,885 participants (Supplementary Material 2, gr.elmerpub.com). These investigations originated from different world regions, including countries from Asia (Japan, China, India, South Korea, Malaysia, Singapore, etc.), Europe (Denmark, Germany, Belgium, Poland), Middle East (Saudi Arabia, Lebanon, Jordan, Bahrain), and the Americas (United States, Colombia, Chile, Peru, among others).
Regarding study design, most opted for a cross-sectional approach, employing both probabilistic and non-probabilistic sampling. Sample size showed considerable variations: from analyses with 193 subjects [19] to much larger samples of 88,607 participants [48].
Concerning sex composition, the proportion of women varied widely, ranging from a minimum of approximately 23% [38] to up to 79% in certain studies [50]. Some publications did not specify the mean age of participants, while others provided averages ranging approximately from 22.7 years [25] to 51.2 years [39].
Sampling methodology also showed differences: some studies selected participants through telephone calls [12, 17], online surveys [34, 51], or health center visits [14, 27]. Others chose to recruit volunteers in specific contexts (e.g., shopping centers or festivals). Additionally, some studies indicated having excluded participants with organic gastrointestinal diseases or alarm symptoms, while others recruited samples from the general population and subsequently discarded incomplete questionnaires or potential cases of concomitant diseases.
Regarding the risk of bias analysis of included studies, generally high methodological quality was found. Studies with probabilistic sampling achieved a quality score of 8, while those with non-probabilistic sampling obtained 7 points, indicating a low risk of bias in both groups. Interestingly, no study reached the maximum score of 9 points, as none conducted a comparative analysis with the non-surveyed group.
Meta-analysis of IBS prevalence - Rome III
This meta-analysis included 26 studies contributing a total of 78,172 participants [10-29, 33, 36-39, 47] (Fig. 2). The estimated global prevalence of IBS, based on Rome III criteria, was 13.21% (95% CI: 10.70-15.94%). The analysis revealed a high degree of heterogeneity (I2 = 99%, P < 0.001).
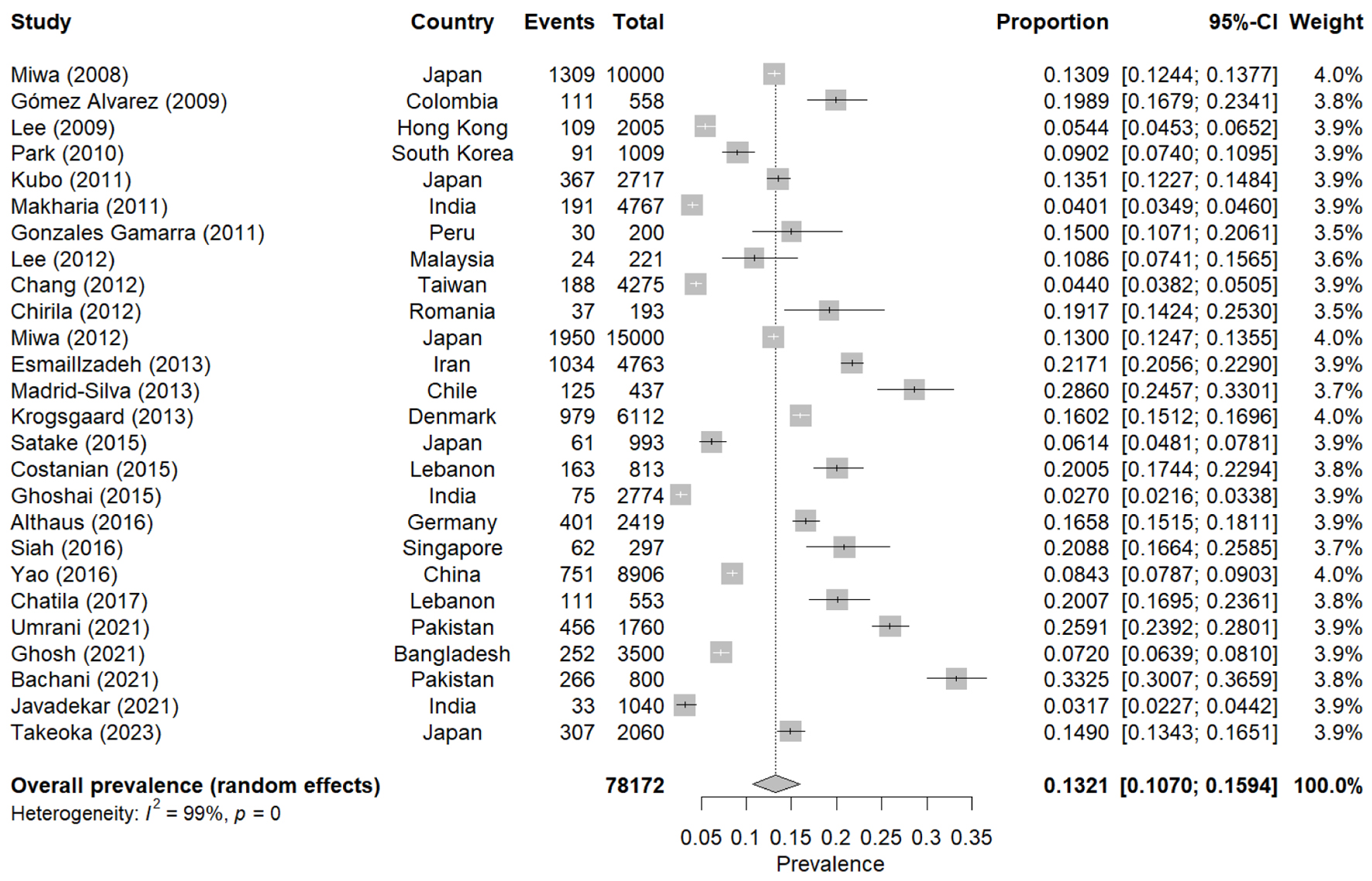 Click for large image | Figure 2. Forest plot of the meta-analysis of the prevalence of IBS - Rome III. IBS: irritable bowel syndrome. |
Individual prevalences showed marked variation, with minimum values close to 2.0% and maximums exceeding 33.0%. Additionally, a notable disparity was observed in study sample sizes, which ranged from 193 participants [19] to 15,000 [20], influencing the statistical weight of each study in the global estimation. Some studies presented larger population samples (e.g., n = 4,767) [15], while others focused on smaller populations or had more restricted inclusion criteria.
Meta-analysis of IBS prevalence - Rome IV
For studies using Rome IV criteria, 17 investigations with 110,713 participants were included [30-32, 34, 35, 40-46, 48-52] (Fig. 3). The estimated global prevalence was 17.14% (95% CI: 12.00-22.99%), with very high heterogeneity (I2 = 100%, P < 0.001).
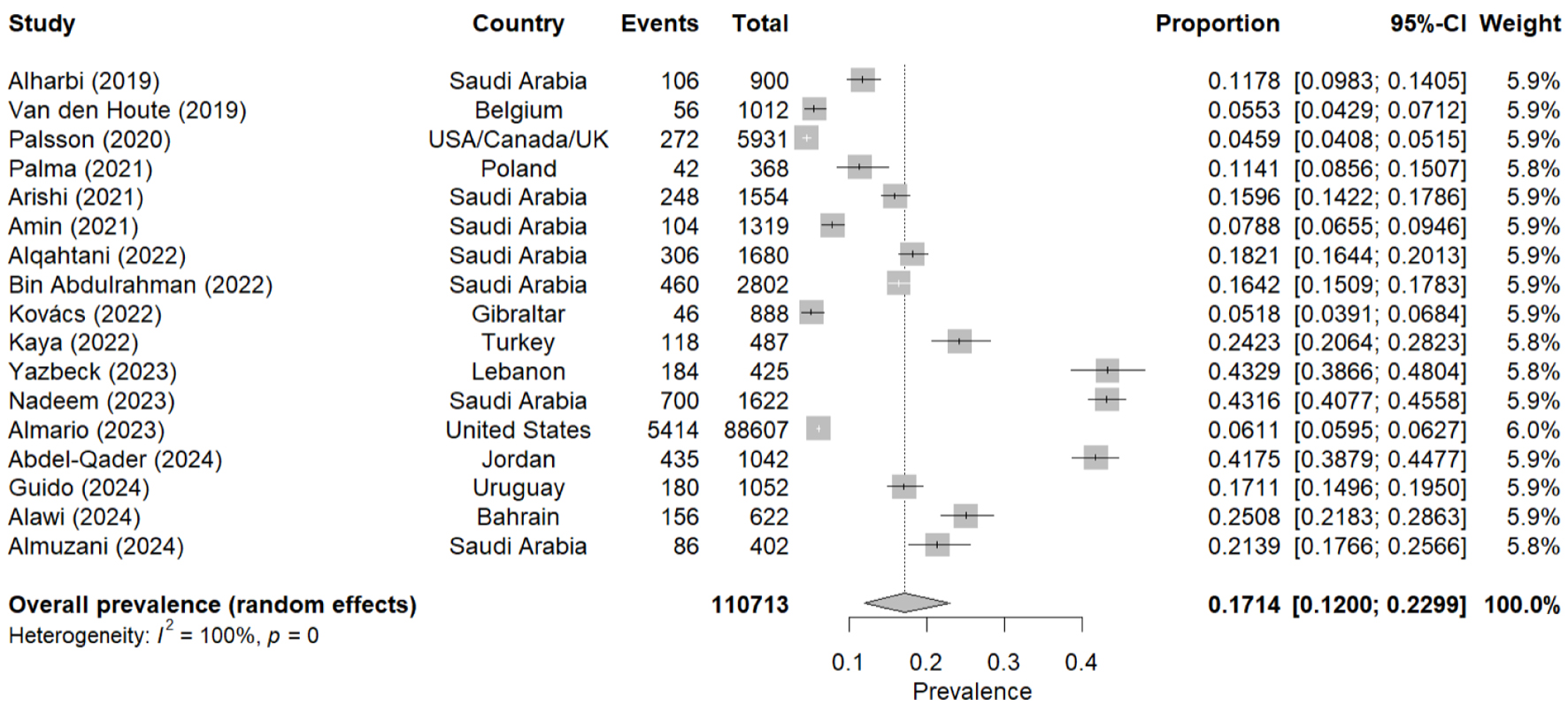 Click for large image | Figure 3. Forest plot of the meta-analysis of the prevalence of IBS - Rome IV. IBS: irritable bowel syndrome. |
Individual prevalences fluctuated from values close to 5.5% [31] to estimates exceeding 43.0% [46]. Sample size also showed considerable differences, notably in a study with 88,607 participants [48], which provided the greatest statistical weight in this meta-analysis. Other studies with fewer subjects (e.g., n = 368) [34] contributed more specific estimates but maintained the trend of high methodological and population variability.
Subgroup analysis: IBS prevalence in studies with probabilistic sampling
In the subgroup analysis based exclusively on studies that employed probabilistic sampling, with 14 studies for Rome III [10-13, 15-19, 23, 28, 36, 39, 47] and nine for Rome IV [30-32, 35, 41, 43, 48, 49, 51], a reduction in prevalence estimates was observed for both diagnostic criteria. The global prevalence for studies using Rome III criteria adjusted to 11.19% (95% CI: 8.55-14.12%; I2 = 99%), while for those using Rome IV, the prevalence was estimated at 13.28% (95% CI: 8.36-19.13%; I2 = 99.8%) (Table 1).
 Click to view | Table 1. Sensitivity Analysis of IBS Prevalence Stratified by Sampling |
Meta-analysis of IBS prevalence by country according to Rome III and IV criteria
IBS prevalence estimates show variations among included countries in studies that applied Rome III and IV criteria (Table 2). In the first group, 18 countries were evaluated, where values ranged from 3.3% (India) to 29.42% (Pakistan) [10-29, 33, 36-39, 47], while in the second group, which evaluated 12 countries, it ranged from 4.59% (USA/Canada/UK) to 43.29% (Lebanon) [30-32, 34, 35, 40-46, 48-52]. This disparity is reflected in the heterogeneity indices (I2), which were elevated in most cases.
 Click to view | Table 2. Global IBS Prevalence According to Rome III and IV Criteria: Analysis by Region or Country |
Furthermore, the number of studies per country varies notably. For example, Japan [10, 14, 20, 24, 47] and Saudi Arabia [30, 35, 40-42, 46, 52] presented multiple investigations within each version of the criteria (Rome III and Rome IV, respectively). At the same time, the remaining countries showed results based on a single study.
Additionally, Figures 4 and 5 show the prevalence distribution by country, both generally and by sex.
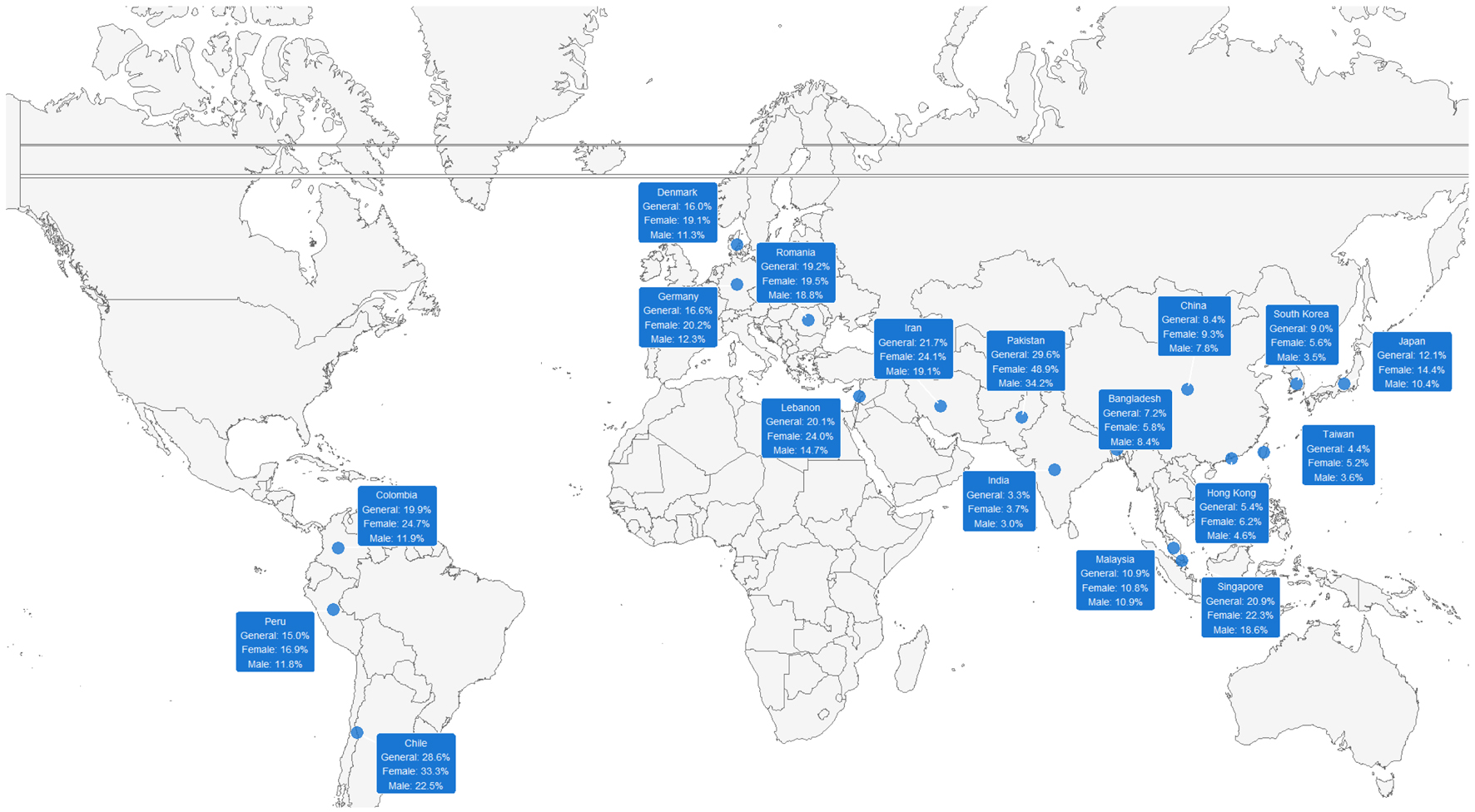 Click for large image | Figure 4. Global distribution of IBS prevalence according to Rome III criteria, stratified by sex. IBS: irritable bowel syndrome. |
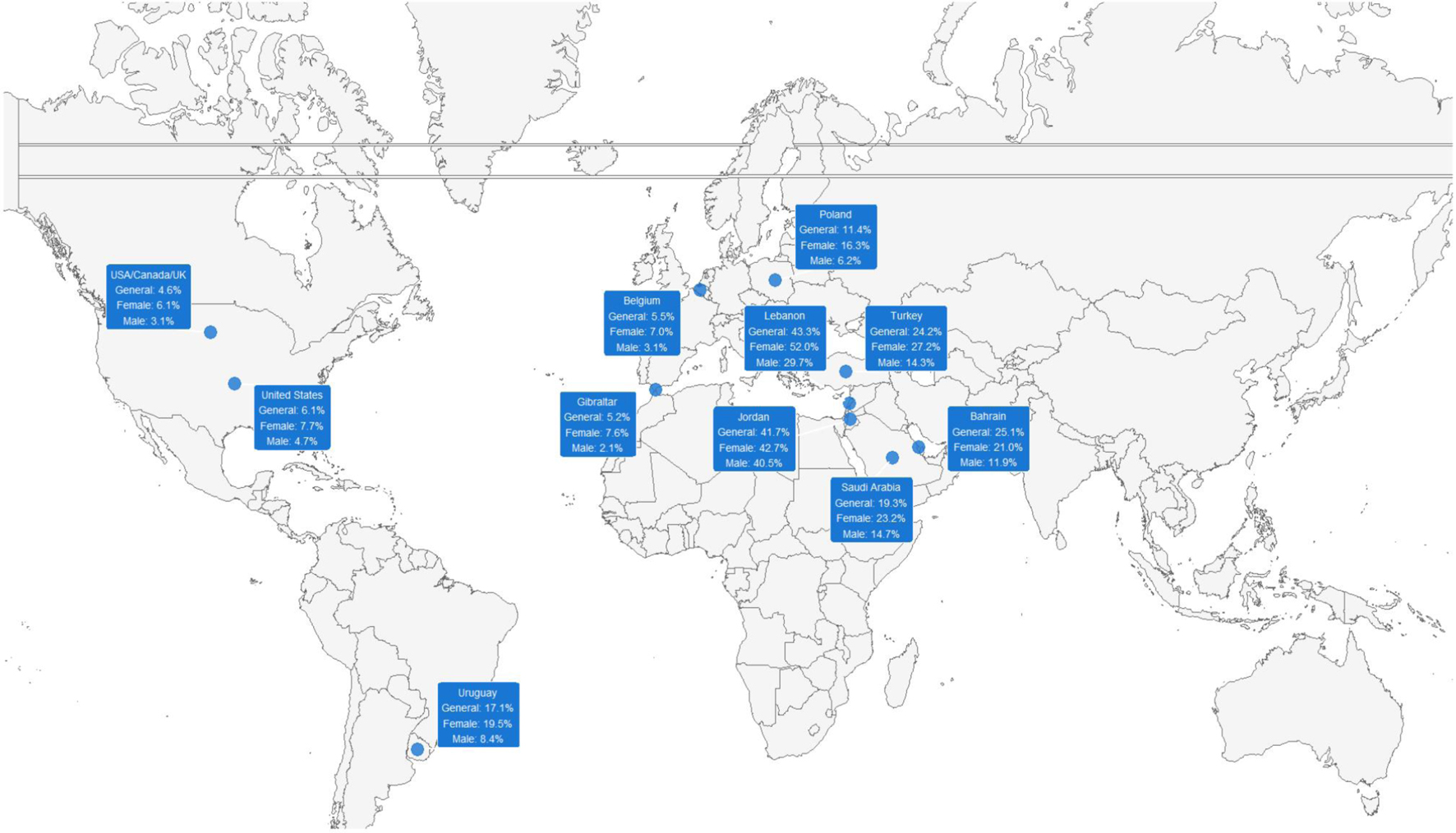 Click for large image | Figure 5. Global distribution of IBS prevalence according to Rome IV criteria, stratified by sex. IBS: irritable bowel syndrome. |
Meta-analysis of global IBS prevalence according to Rome III and IV criteria stratified by sex
The sensitivity analysis conducted to estimate IBS prevalence, differentiated between women and men, included 26 studies based on Rome III [10-29, 33, 36-39, 47] and 17 on Rome IV [30-32, 34, 35, 40-46, 48-52] (Table 3). Under Rome III criteria, the pooled prevalence in women was 15.69% (95% CI: 12.29-19.41%; I2 = 98.9%), while in men, it was 11.10% (95% CI: 8.89-13.52%; I2 = 98.0%).
 Click to view | Table 3. Sensitivity Analysis of IBS Prevalence Stratified by Sex |
In the case of Rome IV, the combined prevalence reached 20.17% (95% CI: 14.48-26.54%; I2 = 99.2%) in women and 11.45% (95% CI: 7.39-16.29%; I2 = 98.9%) in men. In both sets of criteria, a high degree of heterogeneity was observed (I2 > 98%), reflecting the methodological and population diversity of the included studies.
Meta-regression of IBS prevalence according to Rome III and IV criteria by publication year
Figure 6 shows the meta-regression analysis for both Rome III (Fig. 6a) and IV (Fig. 6b) by year of publication. For Rome III, based on 26 studies evaluated during the period 2008 - 2023, no statistically significant temporal trend was observed (P = 0.587), showing a relatively flat regression line over time. Prevalence remains stable around 10-15%, with some outliers such as Madrid-Silva (2013) reporting prevalences close to 30%. The width of the confidence band reflects substantial heterogeneity among studies, indicating that factors other than publication year have greater influence on the observed differences. The size of each bubble corresponds to the sample size, where studies with larger samples (e.g., [10, 20]) have greater statistical weight in the model.
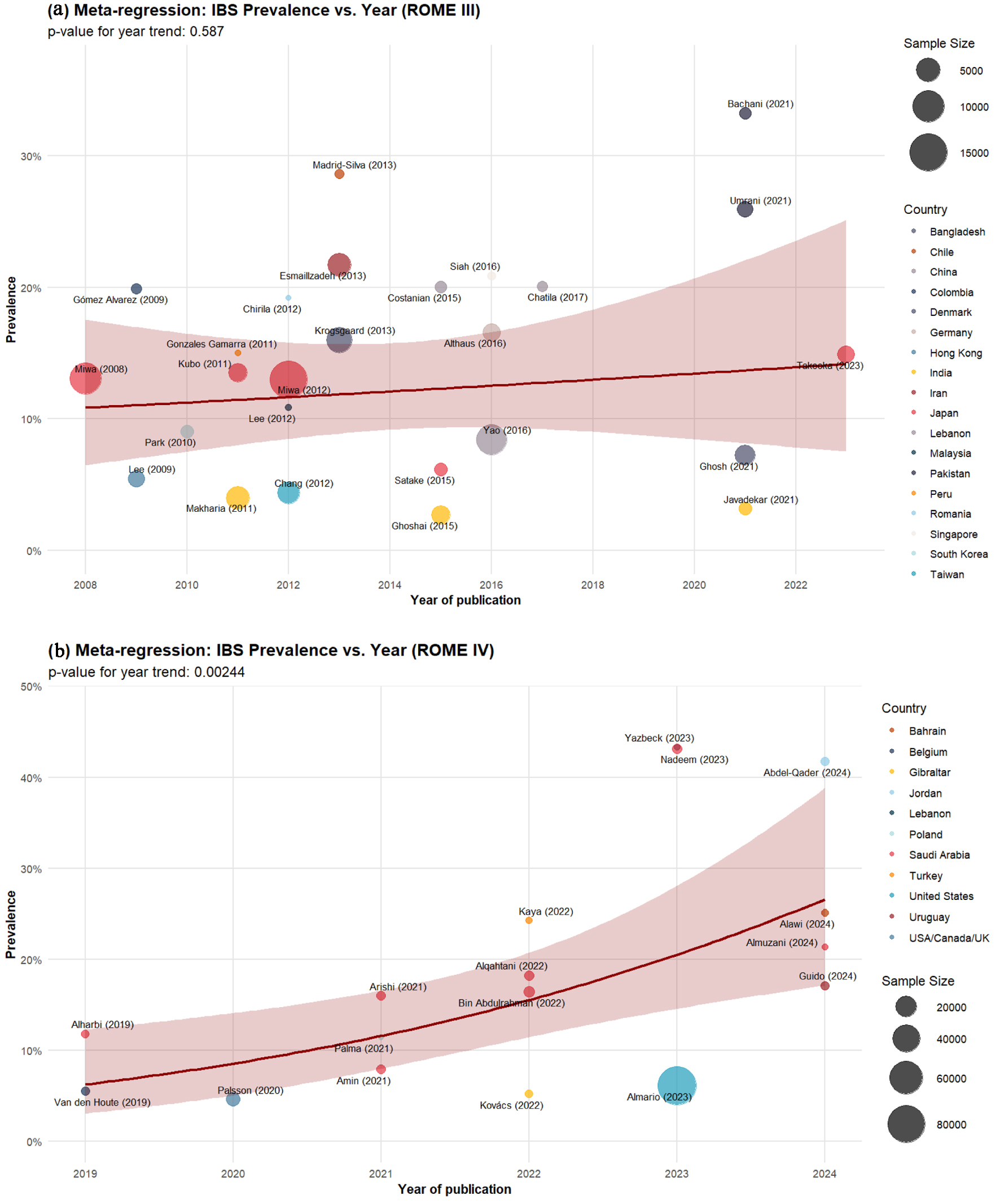 Click for large image | Figure 6. Meta-regression of the prevalence of IBS according to Rome III (a) and IV (b) criteria by year of publication. IBS: irritable bowel syndrome. |
In contrast, the Rome IV analysis, based on 17 studies from the period 2019 - 2024, shows a statistically significant temporal trend (P = 0.00244) with a pronounced upward slope. Prevalence estimates show a notable increase from values of 5-15% in 2019 - 2020 publications [31, 32] to figures of 20-45% in more recent works [45, 46, 49].
Publication bias analysis
Finally, a publication bias analysis was conducted using funnel plots (Supplementary Material 3, gr.elmerpub.com), employing the Freeman-Tukey double arcsine transformation. For studies using Rome III criteria, the funnel plot shows a relatively symmetrical distribution of studies around the estimated mean, with a slight rightward asymmetry, suggesting minimal possible publication bias. Most studies cluster in the upper part of the funnel, indicating adequate precision in the estimates.
Regarding studies that employed Rome IV criteria, the funnel plot shows a more dispersed but relatively symmetrical distribution. Studies are distributed more uniformly along the horizontal axis, with some studies located at the extremes of the graph. While fewer studies are available for Rome IV, the general distribution suggests a low risk of systematic publication bias.
| Discussion | ▴Top |
Main findings
This SR and meta-analysis demonstrates considerable variability in IBS prevalence estimates across countries and between studies employing Rome III and Rome IV criteria. Generally, figures based on Rome III were around 13%, while studies using Rome IV reached approximately 17%. Furthermore, another relevant finding is the high heterogeneity (I2 > 90%) detected in most estimates, suggesting important differences in studied populations, recruitment methods, and how IBS criteria were applied. This variability is also reflected in the meta-regressions by publication year, where upward trends in prevalence are observed, albeit with wide confidence bands. Collectively, these results underscore the complexity of uniformly evaluating IBS at a global level and the need to standardize diagnostic approaches to improve the comparability of future research.
Comparison with other studies
It is important to differentiate these results from the prevalence study published in 2020. Unlike Oka et al [5], our SR applied stricter selection criteria to ensure higher methodological quality and reduce the risk of bias. First, we only included primary observational studies published in peer-reviewed journals, excluding conference abstracts and gray literature that might lack important methodological details. This is why we have fewer studies in total than the 57 included in the previous review, of which several were abstracts, such as Amieva-Balmori et al, 2014 [53], Palsson et al, 2016 [54], and Kumar et al, 2019 [55], which could have affected the quality and reliability of their estimates.
Moreover, while the previous SR included studies that approximated Rome III or IV criteria, our review was limited to studies that used validated Rome III and IV questionnaires in their original form. This methodological decision was based on the fact that approximations could overestimate IBS prevalence, as evidenced in their results where the pooled prevalence was higher in studies that approximated Rome III criteria (14.0%) compared to those that used the validated questionnaire (8.4%) [5]. This substantial difference highlights the importance of strictly adhering to validated instruments to obtain more precise and comparable estimates of IBS prevalence.
Furthermore, a particularly relevant finding of our current SR is the substantial difference in prevalence estimates using Rome IV criteria. While the previous one found a global prevalence of 3.8% (based on only six studies), our current review, with a significantly larger number of studies, reveals a global prevalence of 17.14% (or 13.28% when limited to studies with probabilistic sampling). This marked difference could be explained not only by the larger number of studies included in our analysis but also by the evolution in understanding and application of Rome IV criteria in clinical practice and research. Thus, our findings challenge the previous notion that Rome IV criteria are more restrictive and result in lower prevalence rates, suggesting that the true prevalence of IBS might be significantly higher than previously thought.
Explanation of results
The observed differences in prevalence between studies that applied Rome III (13.21%) and Rome IV (17.14%) criteria represent an intriguing finding that deserves detailed analysis. At first glance, this might seem counterintuitive, given that Rome IV introduces stricter criteria, with greater emphasis on abdominal pain as a central symptom of IBS and adjustments in the temporal intervals of symptom presentation. However, this apparent paradox can be explained through various methodological and contextual factors that characterize the studies included in our review.
A crucial factor is the temporal and geographical context of the analyzed studies. Research using Rome IV was conducted more recently, during a period of greater awareness about functional gastrointestinal disorders, and concentrated in regions where traditionally higher IBS figures are reported, such as the Middle East. Additionally, these studies more frequently employed modern data collection methodologies, such as online surveys and digital tools, which could facilitate the recruitment of certain population groups, particularly in urban settings and those with higher educational levels.
Fundamental changes in the definition and frequency of the cardinal symptom can also explain the observed differences. Rome III [56] used a broader definition that included both abdominal “pain” and “discomfort,” with a required frequency of at least 3 days per month in the last 3 months. Although more inclusive when considering discomfort, this definition might have generated ambiguity in symptom interpretation and reporting, given that “discomfort” can be understood differently according to cultural and linguistic context.
Rome IV [4] simplified the cardinal criterion by focusing exclusively on “abdominal pain,” eliminating the term “discomfort,” but modifying the required frequency to at least 1 day per week in the last 3 months. This modification might facilitate case identification for two reasons: the specificity of the term “pain” allows a more uniform and recognizable interpretation by patients, and weekly frequency might be easier to remember and report than monthly frequency, thus improving self-reporting accuracy.
A particularly relevant finding emerges when restricting the evaluation to studies that employed exclusively probabilistic sampling, where we observe that prevalence with Rome III adjusts to 11.19% and with Rome IV to 13.28%. This more modest difference between both criteria suggests that studies with probabilistic sampling likely offer a more precise and representative estimate of the true IBS prevalence in the general population and that selection biases might influence the larger disparity observed in the global analysis in studies with non-probabilistic sampling.
These observations suggest that the differences in prevalence between Rome III and IV reflect changes in diagnostic criteria per se and an evolution in the understanding, recognition, and methodology of studying IBS. For future research, establishing standardized protocols that control these methodological and contextual factors will be crucial, thus allowing a more precise evaluation of the real impact of different diagnostic criteria in estimating IBS prevalence.
Additionally, it is important to mention that multiple interrelated factors can explain the trend toward increased IBS prevalence observed in the temporal meta-regression. On one hand, there might be greater awareness in the medical community and the general population about functional gastrointestinal disorders, leading to better recognition and reporting of symptoms. Broader access to medical information through digital media and health campaigns has contributed to people identifying and seeking medical attention for symptoms that previously might have been ignored or normalized. Since these are still researchers’ assumptions, further studies would be needed to confirm these findings.
Differences found by sex and country
In the present review, notable discrepancies have been identified in IBS prevalence among various countries, spanning regions as diverse as Asia, Europe, North America, and the Middle East. For example, studies conducted in Lebanon and Jordan report particularly high prevalences, while in East Asian areas (Hong Kong, Taiwan, or China), significantly lower figures are found. This variability may be due, in part, to differences in food culture, lifestyles, and psychosocial factors, as well as the availability and use of diagnostic resources in each region [7, 57]. Furthermore, recruitment characteristics and how Rome criteria (III or IV) are applied also influence the obtained estimates, contributing to high heterogeneity among studies.
Another constant in the IBS field is the higher prevalence in women compared to men, a finding corroborated by the previous meta-analysis [5]. Different investigations have proposed pathophysiological mechanisms to explain this pattern, specifically in females. Among them, hormonal fluctuations, particularly estrogen and progesterone levels, can modulate intestinal motility and visceral sensitivity [3, 58]. Additionally, it has been suggested that women might more frequently experience anxiety or stress reactions about digestive symptoms, increasing the bidirectional communication of the gut-brain axis and facilitating the persistence or exacerbation of abdominal pain [1, 2].
IBS is considered a functional gastrointestinal disorder of multifactorial etiology. It involves a complex interaction between intestinal microbiota, visceral hypersensitivity, enteric nervous system dysfunctions, and psychosocial factors [1, 57]. Thus, higher prevalence figures might manifest in populations with high-stress levels or greater exposure to irritating dietary factors. In women, sex hormones can modulate intestinal permeability and low-grade inflammation, increasing susceptibility to developing alterations in motility and pain perception [3]. Additionally, there are cultural and social factors that can condition symptom presentation, subjective reporting, and healthcare-seeking behavior, which, in turn, influence IBS detection.
Public health significance of findings
The results of this meta-analysis demonstrate that IBS constitutes a global health problem, given its high prevalence across multiple regions and its tendency to be more frequent in women. Understanding the true magnitude of the disease is fundamental for health policy formulation, especially in countries where the economic and social burden of functional gastrointestinal disorders tends to be underestimated. The high heterogeneity found in studies indicates that intervention strategies should be adjusted to the particularities of each region and population.
In terms of public health, IBS carries a significant socioeconomic impact, associated with both direct medical costs (consultations, diagnostic tests, medications) and indirect costs (work absenteeism, reduced productivity) [59]. Identifying groups with greater susceptibility - by sex, age, or geographical region - facilitates the design of targeted prevention and control programs. Moreover, the diversity of IBS clinical manifestations requires the implementation of timely diagnostic protocols and incorporating multidisciplinary approaches (nutrition, psychology, gastroenterology) in primary care systems.
The verification of differences between Rome III and Rome IV criteria underscores the need for healthcare professionals to be trained and updated regarding the latest diagnostic guidelines. This helps minimize underdiagnosis or misdiagnosis, avoiding overmedication and excessive use of healthcare resources. Additionally, the higher prevalence found in women highlights the importance of integrating sex perspective when formulating preventive and therapeutic interventions, considering that women might present specific hormonal and psychosocial factors that influence the severity and chronicity of the condition [1, 57].
Finally, our findings emphasize the urgent need to develop prevalence studies in world regions with a notable scarcity of data, particularly in Africa, Eastern Europe, and much of Central Asia. Promoting multinational collaborative research using standardized methodologies and uniform diagnostic criteria is essential, allowing for generating comparable data and developing guidelines adapted to different sociocultural contexts. Integrating research networks could facilitate obtaining more representative data and identifying global patterns in IBS prevalence.
Study strengths and limitations
One of the main strengths of this review is the inclusion of a considerable number of studies from diverse regions, allowing a broad perspective of IBS prevalence at a global level. Moreover, applying standardized protocols (PRISMA) and specific tools for prevalence studies provides methodological rigor and transparency in article selection. On the other hand, the high heterogeneity (I2) found in the meta-analyses represents an important limitation, suggesting substantial variations in population, recruitment methods, and how diagnostic criteria are applied. Additionally, some multinational studies reported combined prevalence data for multiple countries (e.g., USA/Canada/UK), which precluded country-specific analyses and may have masked regional differences. The lack of uniformity in presenting additional data to understand disparities (e.g., dietary habits, comorbidities) may also limit a deeper understanding of the findings.
Conclusions and recommendations
The findings of this SR and meta-analysis confirm that IBS is a frequent disorder globally. The estimated combined prevalence was 13.21% (95% CI: 10.70-15.94%) with Rome III criteria and 17.14% (95% CI: 12.00-22.99%) with Rome IV. However, when considering only studies with probabilistic sampling, these figures decreased to approximately 10% and 13%, respectively. Additionally, a higher percentage of cases was observed in women, which aligns with most previous studies on the topic. Nevertheless, despite the high heterogeneity among analyzed works, this overview provides solid evidence of the need for a more homogeneous diagnostic and therapeutic approach adapted to each population’s reality.
Regarding clinical practice and public health, conducting more IBS prevalence studies, especially in underrepresented regions, and using rigorous methodologies is imperative. Future studies should employ standardized protocols and probabilistic sampling, ensuring consistent application of Rome criteria to obtain more precise estimates. Particular attention is required in adequately characterizing studied populations, including a gender perspective approach and considering relevant sociodemographic variables that could influence prevalence. Furthermore, it is essential to establish collaborative networks among research centers to develop multicenter studies that allow valid comparisons between different regions and cultural contexts.
In parallel, it is proposed to strengthen healthcare personnel training programs in applying diagnostic criteria and promote educational initiatives directed at the general population and risk groups. The evidence generated by new prevalence studies will be crucial for designing health policies and clinical guidelines that effectively address the global burden of IBS, considering the particularities of each region and population.
| Supplementary Material | ▴Top |
Suppl 1. Search strategy.
Suppl 2. Summary of prevalence studies of irritable bowel syndrome.
Suppl 3. Publication bias analysis using funnel plots for IBS prevalence studies according to Rome III (A) and Rome IV (B) criteria.
Acknowledgments
Special thanks to the members of Universidad Nacional Toribio Rodriguez de Mendoza de Amazonas (UNTRM), Amazonas, Peru, for their support and contributions throughout the completion of this research.
Financial Disclosure
This study was funded by the Vicerectorado de Investigacion of the Universidad Nacional Toribio Rodriguez de Mendoza de Amazonas.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Since this is a secondary data analysis, informed consent was not required.
Author Contributions
Jhosmer Ballena-Caicedo: conceptualization, investigation, methodology, writing - original draft, writing - review and editing; Lupita Ana Maria Valladolid-Sandoval: methodology, data curation, writing - original draft, writing - review and editing; Fiorella E. Zuzunaga-Montoya: software, investigation, funding acquisition, resources, data curation, methodology, writing - original draft, writing - review and editing; Victor Juan Vera-Ponce: conceptualization, investigation, formal analysis, methodology, resources, writing - original draft, writing - review and editing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology. 2016;150(6):1262-1279.e2.
doi pubmed - Lacy BE, Patel NK. Rome criteria and a diagnostic approach to irritable bowel syndrome. J Clin Med. 2017;6(11):99.
doi pubmed - Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel disorders. Gastroenterology. 2016;150(6):1393-1407.e5.
doi pubmed - Palsson OS, Whitehead WE, van Tilburg MA, Chang L, Chey W, Crowell MD, Keefer L, et al. Rome IV diagnostic questionnaires and tables for investigators and clinicians. Gastroenterology. 2016;150(6):1481-1491.
doi pubmed - Oka P, Parr H, Barberio B, Black CJ, Savarino EV, Ford AC. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(10):908-917.
doi pubmed - Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J, Whitehead WE, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome foundation global study. Gastroenterology. 2021;160(1):99-114.e113.
doi pubmed - Black CJ, Ford AC. Global burden of irritable bowel syndrome: trends, predictions and risk factors. Nat Rev Gastroenterol Hepatol. 2020;17(8):473-486.
doi pubmed - Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
doi pubmed - Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13(3):147-153.
doi pubmed - Miwa H. Prevalence of irritable bowel syndrome in Japan: Internet survey using Rome III criteria. Patient Prefer Adherence. 2008;2:143-147.
pubmed - Gomez Alvarez DF, Morales Vargas JG, Rojas Medina LM, Mujica Oviedo SC, Camacho Lopez PA, Rueda Jaimes GE. [Prevalence of irritable bowel syndrome and associated factors according to the Rome III diagnostic criteria in a general population in Colombia]. Gastroenterol Hepatol. 2009;32(6):395-400.
doi pubmed - Lee S, Wu J, Ma YL, Tsang A, Guo WJ, Sung J. Irritable bowel syndrome is strongly associated with generalized anxiety disorder: a community study. Aliment Pharmacol Ther. 2009;30(6):643-651.
doi pubmed - Park DW, Lee OY, Shim SG, Jun DW, Lee KN, Kim HY, Lee HL, et al. The Differences in Prevalence and Sociodemographic Characteristics of Irritable Bowel Syndrome According to Rome II and Rome III. J Neurogastroenterol Motil. 2010;16(2):186-193.
doi pubmed - Kubo M, Fujiwara Y, Shiba M, Kohata Y, Yamagami H, Tanigawa T, Watanabe K, et al. Differences between risk factors among irritable bowel syndrome subtypes in Japanese adults. Neurogastroenterol Motil. 2011;23(3):249-254.
doi pubmed - Makharia GK, Verma AK, Amarchand R, Goswami A, Singh P, Agnihotri A, Suhail F, et al. Prevalence of irritable bowel syndrome: a community based study from northern India. J Neurogastroenterol Motil. 2011;17(1):82-87.
doi pubmed - Gamarra RGG, Sanchez JGR, Jimenez FL, Benavides FC, Velez CD. Prevalencia del Sindrome de Intestino Irritable en la Poblacion Adulta de Chiclayo durante el ano 2011. Rev Gastroenterol Peru. 2012;381-386.
doi - Lee YY, Waid A, Tan HJ, Chua AS, Whitehead WE. Rome III survey of irritable bowel syndrome among ethnic Malays. World J Gastroenterol. 2012;18(44):6475-6480; discussion p 6479.
doi pubmed - Chang FY, Chen PH, Wu TC, Pan WH, Chang HY, Wu SJ, Yeh NH, et al. Prevalence of functional gastrointestinal disorders in Taiwan: questionnaire-based survey for adults based on the Rome III criteria. Asia Pac J Clin Nutr. 2012;21(4):594-600.
pubmed - Chirila I, Petrariu FD, Ciortescu I, Mihai C, Drug VL. Diet and irritable bowel syndrome. J Gastrointestin Liver Dis. 2012;21(4):357-362.
pubmed - Miwa H. Life style in persons with functional gastrointestinal disorders—large-scale internet survey of lifestyle in Japan. Neurogastroenterol Motil. 2012;24(5):464-471.e217.
doi pubmed - Esmaillzadeh A, Keshteli AH, Hajishafiee M, Feizi A, Feinle-Bisset C, Adibi P. Consumption of spicy foods and the prevalence of irritable bowel syndrome. World J Gastroenterol. 2013;19(38):6465-6471.
doi pubmed - Madrid-Silva AM, Defilippi-Caffri C, Landskron-Ramos G, Olguin-Herrera F, Reyes-Ponce A, Castro-Lara A, Larrain-Corp S, et al. [The prevalence of irritable bowel symptoms in a population of shopping mall visitors in Santiago de Chile]. Rev Gastroenterol Mex. 2013;78(4):203-210.
doi pubmed - Krogsgaard LR, Engsbro AL, Bytzer P. The epidemiology of irritable bowel syndrome in Denmark. A population-based survey in adults </=50 years of age. Scand J Gastroenterol. 2013;48(5):523-529.
doi pubmed - Satake R, Sugawara N, Sato K, Takahashi I, Nakaji S, Yasui-Furukori N, Fukuda S. Prevalence and predictive factors of irritable bowel syndrome in a community-dwelling population in Japan. Intern Med. 2015;54(24):3105-3112.
doi pubmed - Costanian C, Tamim H, Assaad S. Prevalence and factors associated with irritable bowel syndrome among university students in Lebanon: findings from a cross-sectional study. World J Gastroenterol. 2015;21(12):3628-3635.
doi pubmed - Ghoshal UC, Singh R. Frequency and risk factors of functional gastro-intestinal disorders in a rural Indian population. J Gastroenterol Hepatol. 2017;32(2):378-387.
doi pubmed - Althaus A, Broicher W, Wittkamp P, Andresen V, Lohse AW, Lowe B. Determinants and frequency of irritable bowel syndrome in a German sample. Z Gastroenterol. 2016;54(3):217-225.
doi pubmed - Siah KT, Wong RK, Chan YH, Ho KY, Gwee KA. Prevalence of irritable bowel syndrome in Singapore and its association with dietary, lifestyle, and environmental factors. J Neurogastroenterol Motil. 2016;22(4):670-676.
doi pubmed - Chatila R, Merhi M, Hariri E, Sabbah N, Deeb ME. Irritable bowel syndrome: prevalence, risk factors in an adult Lebanese population. BMC Gastroenterol. 2017;17(1):137.
doi pubmed - Alharbi SH, Alateeq FA, Alshammari KI, Ahmed HG, Alharbi SH, Alateeq FA, et al. IBS common features among Northern Saudi population according to Rome IV criteria. AIMS Med Sci. 2019;6(2):148-157.
doi - Van den Houte K, Carbone F, Pannemans J, Corsetti M, Fischler B, Piessevaux H, Tack J. Prevalence and impact of self-reported irritable bowel symptoms in the general population. United European Gastroenterol J. 2019;7(2):307-315.
doi pubmed - Palsson OS, Whitehead W, Tornblom H, Sperber AD, Simren M. Prevalence of Rome IV functional bowel disorders among adults in the United States, Canada, and the United Kingdom. Gastroenterology. 2020;158(5):1262-1273.e1263.
doi pubmed - Umrani S, Jamshed W, Rizwan A. Association between psychological disorders and irritable bowel syndrome. Cureus. 2021;13(4):e14513.
doi pubmed - Palma J, Antoniewicz J, Borecki K, Tejchman K, Skonieczna-Zydecka K, Maciejewska-Markiewicz D, Ryterska K, et al. Irritable bowel syndrome prevalence among participants of Woodstock rock festival in Poland based on Rome IV criteria questionnaire. Int J Environ Res Public Health. 2021;18(21):11464.
doi pubmed - Arishi AM, Elmakki EE, Hakami OM, Alganmy OM, Maashi SM, Al-Khairat HK, Sahal YA, et al. Irritable bowel syndrome: prevalence and risk factors in Jazan Region, Saudi Arabia. Cureus. 2021;13(6):e15979.
doi pubmed - Ghosh DK, Nath M, Biswas A, Khondakar MFA, Ghosh CK. Prevalence of irritable bowel syndrome: A comparison between rural and urban settings in Bangladesh: IBS among rural and urban population. Bangladesh Med Res Counc Bull. 2021;47(1):70-77.
doi - Bachani P, Kumar L, Kumar N, Fatima M, Naz S, Memon MK, Memon S, et al. Prevalence of irritable bowel syndrome and frequency of symptoms in the general population of Pakistan. Cureus. 2021;13(1):e12541.
doi pubmed - Javadekar NS, Oka GA, Joshi AS, Vaste P, Tamane S, Lawate PS. Prevalence of irritable bowel syndrome and metabolic syndrome among young adults in an annual health check-up setting. JGH Open. 2021;5(10):1148-1153.
doi pubmed - Yao X, Yang YS, Cui LH, Sun G, Peng LH, Wang WF, Hyder Q, et al. The overlap of upper functional gastrointestinal disorders with irritable bowel syndrome in Chinese outpatients: A multicenter study. J Gastroenterol Hepatol. 2016;31(9):1584-1593.
doi pubmed - Amin HS, Irfan F, Karim SI, Almeshari SM, Aldosari KA, Alzahrani AM, Almogbel AT, et al. The prevalence of irritable bowel syndrome among Saudi population in Riyadh by use of Rome IV criteria and self-reported dietary restriction. Saudi J Gastroenterol. 2021;27(6):383-390.
doi pubmed - Alqahtani NH, Mahfouz MEM. The prevalence and risk factors of irritable bowel syndrome in Saudi Arabia in 2019. Int J Prev Med. 2022;13:13.
doi pubmed - Bin Abdulrahman KA, Alenazi NS, Albishri SB, Alshehri FF. Association of migraine and irritable bowel syndrome in Saudi Arabia: a nationwide survey. Biomed Res Int. 2022;2022:8690562.
doi pubmed - Kovacs DB, Szekely A, Hubai AG, Palsson O. Prevalence, epidemiology and associated healthcare burden of Rome IV irritable bowel syndrome and functional dyspepsia in the adult population of Gibraltar. BMJ Open Gastroenterol. 2022;9(1):e000979.
doi pubmed - Kaya YD, Uzuner A. The relationship between abdominal obesity and irritable bowel syndrome in adults. Marmara Med J. 2022;35(1):31-35.
doi - Yazbeck G, Malaeb D, Shaaban H, Sarray El Dine A, Hallit S, Hallit R. Irritable bowel syndrome (IBS) among Lebanese adults: unidentified IBS and associated factors. BMC Public Health. 2023;23(1):1589.
doi pubmed - Nadeem M, Alshahrani SMS, Bin Rakhis RA, Khalban ABA, Alshahrani NAS, Al-Rashdi MHH, et al. Prevalence of irritable bowel syndrome, functional dyspepsia and their overlap in Saudi Arabia. Bahrain Medical Bulletin. 2023;45(1):1-5.
- Takeoka A, Kimura T, Hara S, Hamaguchi T, Fukudo S, Tayama J. Prevalence of irritable bowel syndrome in Japan, China, and South Korea: an international cross-sectional study. J Neurogastroenterol Motil. 2023;29(2):229-237.
doi pubmed - Almario CV, Sharabi E, Chey WD, Lauzon M, Higgins CS, Spiegel BMR. Prevalence and burden of illness of Rome IV irritable bowel syndrome in the United States: results from a nationwide cross-sectional study. Gastroenterology. 2023;165(6):1475-1487.
doi pubmed - Abdel-Qader D. Irritable Bowel Syndrome (IBS) among jordanian adults: uncovering the underdiagnosed and the triggering factors. Natl J Community Med. 2024;15(02):112-120.
doi - Guido V, Pontet Y, Lopez V, Olano C. Prevalencia de sindrome del intestino irritable y otros trastornos funcionales intestinales en Uruguay. Rev Gastroenterol Mexico. 2024;89(2):258-264.
doi - Alawi Z, AlMakna W, Hassan F, Faisal M, Matar H, Alsayyad AS. Prevalence of isolated irritable bowel syndrome among adults in the Kingdom of Bahrain. Cureus. 2024;16(3):e56155.
doi pubmed - Almuzaini AS, Almuzaini R, Alsaleem HN, Alsuhaibani A, Alsohaibani A, Alwehaibi R, Alharbi L, et al. Prevalence and associated risk factors of irritable bowel syndrome among general population: a cross-sectional study in Qassim region, Saudi Arabia. Cureus. 2024;16(4):e57493.
doi pubmed - Amieva-Balmori M, Meixueiro A, Canton P, Remes-Troche JM. Prevalence of irritable bowel syndrome in Mexico. A nationwide population based study using the ROME III questionnaire. Gastroenterology. 2014;146(5):S535.
doi - Palsson OS, Heymen S, Whitehead WE. Non-gastrointestinal pain is increased in irritable bowel syndrome (IBS) but does not account for abdominal pain. Gastroenterology. 2015;148(4):S780.
doi - Kumar Ghosh D, Nath M, Biswas A, Safwath SARP. Prevalence of irritable bowel syndrome: a comparison between rural and urban setting in Bangladesh. J Gastroenterol Hepatol 2016;31(suppl 3):159.
- Development and Validation of Rome III Questionnaire - 2006 [Internet]. Rome Foundation. [citado el 8 de enero de 2025]. Disponible en: https://theromefoundation.org/programs-projects/research-program/development-and-validation-of-rome-iii-questionnaire-2006/.
- Ford AC, Lacy BE, Talley NJ. Irritable Bowel Syndrome. N Engl J Med. 2017;376(26):2566-2578.
doi pubmed - JohnBritto JS, Di Ciaula A, Noto A, Cassano V, Sciacqua A, Khalil M, Portincasa P, et al. Gender-specific insights into the irritable bowel syndrome pathophysiology. Focus on gut dysbiosis and permeability. Eur J Intern Med. 2024;125:10-18.
doi pubmed - Nellesen D, Yee K, Chawla A, Lewis BE, Carson RT. A systematic review of the economic and humanistic burden of illness in irritable bowel syndrome and chronic constipation. J Manag Care Pharm. 2013;19(9):755-764.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.