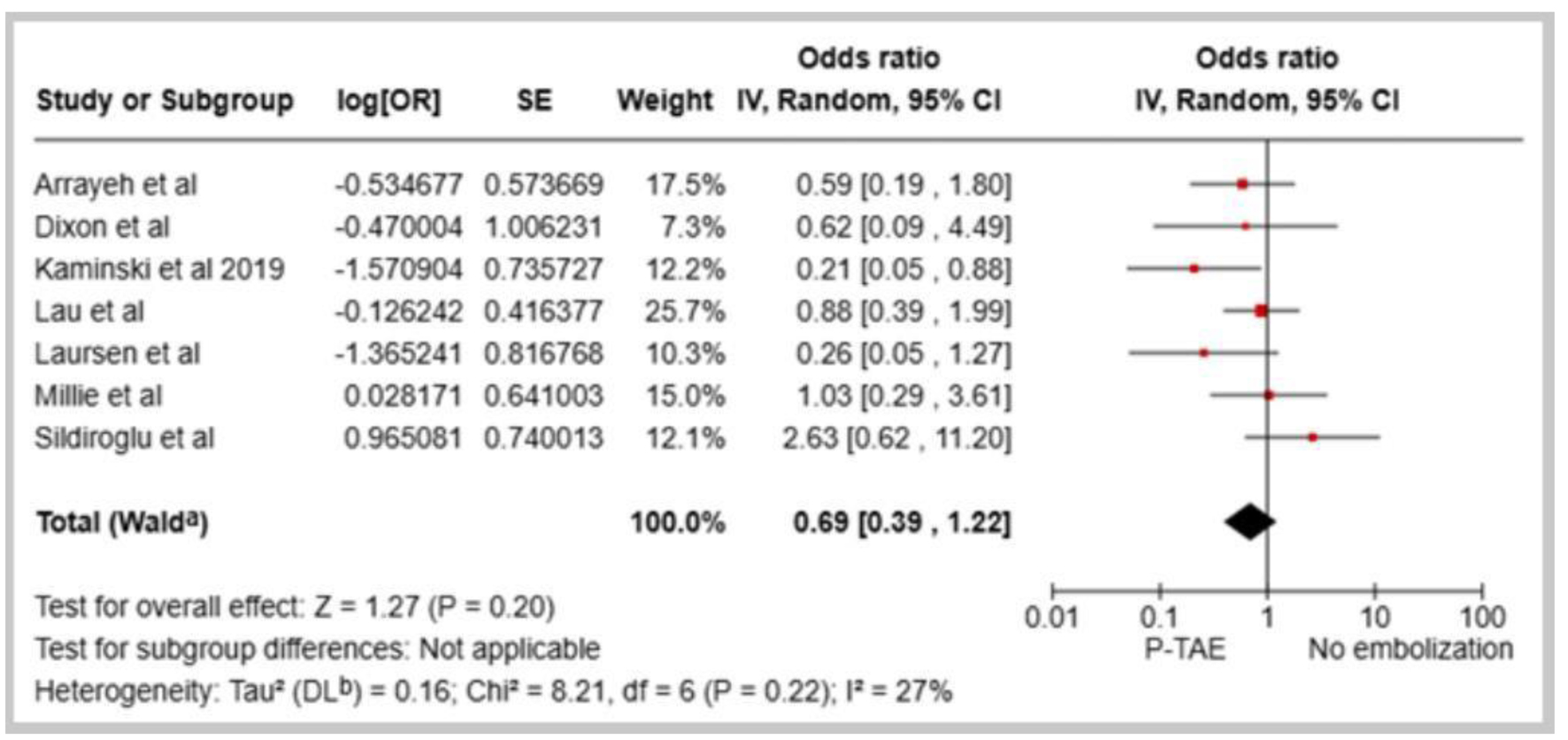
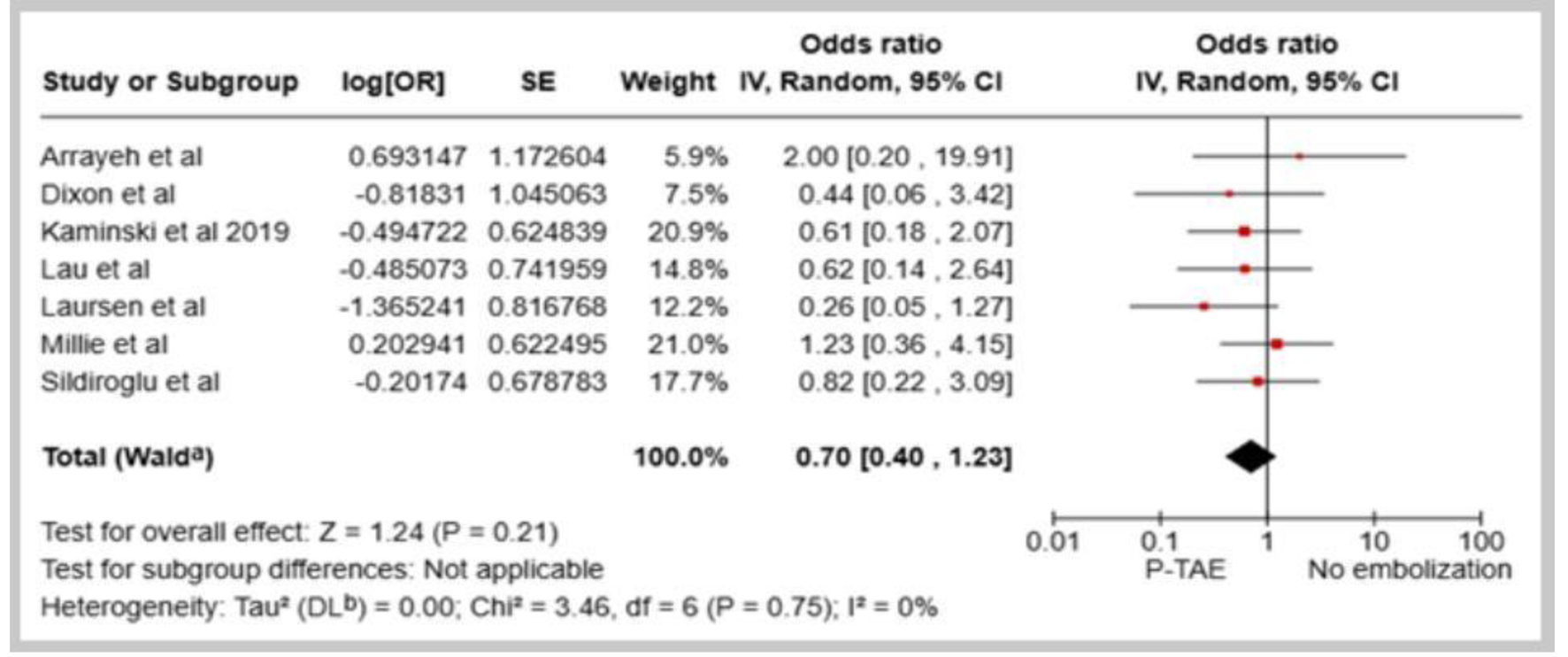
Figure 1. Forest plot of overall rebleeding rate in comparison between prophylactic transcatheter arterial embolization (P-TAE) and no embolization.
| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://gr.elmerpub.com |
Original Article
Volume 18, Number 3, June 2025, pages 139-148
Comparison of Prophylactic Transcatheter Arterial Embolization and Standard Therapy in High-Risk Non-Variceal Upper Gastrointestinal Bleeding: A Meta-Analysis
Figures


Table
| Study | Design | Country | Year of study | Definition of high-risk gastrointestinal bleeding | Study groups, N (%) | Forrest classification (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NE | P-TAE | TAE | Ia | Ib | IIa | IIb | |||||
| P-TAE: prophylactic transcatheter arterial embolization; NE: no embolization in the absence of angiographic evidence of bleeding; TAE: therapeutic arterial embolization; NVUGIB: non-variceal upper gastrointestinal bleeding. | |||||||||||
| Padia et al [12] | Retrospective study | United States | 2009 | Initial endoscopy fails to arrest the NVUGIB. | - | 72 (67) | 36(33) | - | - | - | - |
| Ichiro et al [13] | Retrospective study | Japan | 2011 | Persistent and substantial NVUGIB and hemodynamic instability despite endoscopic intervention. | - | 36 (61) | 23(39) | - | - | - | - |
| Arrayeh et al [14] | Retrospective study | Israel, United States | 2012 | Initial endoscopy fails to arrest the NVUGIB. | 17 (14.7) | 56 (48.7) | 42(36.6) | - | - | - | - |
| Dixon et al [15] | Retrospective study | UK | 2012 | Initial endoscopy fails to arrest the NVUGIB. | 7 (17.5) | 20 (50) | 13(32.5) | - | - | - | - |
| Laursen et al [16] | Randomized controlled trial | Denmark | 2013 | Bleeding from ulcers classified as Forrest I-IIb. | 68 (70.5) | 31 (29.5) | - | 10 | 32 | 50 | 7 |
| Sildiroglu et al [17] | Retrospective study | United States, Turkey | 2014 | Initial endoscopy fails to arrest the NVUGIB. | 22 (29.7) | 18 (24.3) | 31 (41.9) | - | - | - | - |
| Mille et al [18] | Retrospective study | Germany | 2014 | If patients exhibited at least 1 endoscopic as well as 1 clinical risk factor, then they were defined as high-risk patients. | 47 (40) | 55 (47) | 15 (13) | 19 (16) | 39 (33) | 14 (12) | 10 (9) |
| Kaminskis et al 2017 [19] | Prospective Study | Latvia | 2017 | Forrest I-IIb type of ulcer and the Rockall score ≥ 5. | 50 (66.7) | 25 (33.3) | - | 5 (20) | 4 (16) | 11 (44) | 5 (20) |
| Lau et al [20] | Randomized controlled trial | Hong Kong, Thailand, Netherlands, China | 2018 | Patients with actively bleeding gastroduodenal ulcers (Forrest type I) or ulcers with non-bleeding visible vessels (Forrest IIa). | 123 (51) | 118 (49) | - | 42 (17.3) | 90 (37.4) | 109 (45.2) | 0 |
| Kaminskis et al 2019 [21] | Prospective study | Latvia | 2019 | Patients with Forrest Ia-IIc ulcers and the Rockall score ≥ 6. | 341 (85.5) | 58 (14.5) | - | 6 (10.3) | 8 (13.8) | 22 (37.9) | 22 (37.9) |