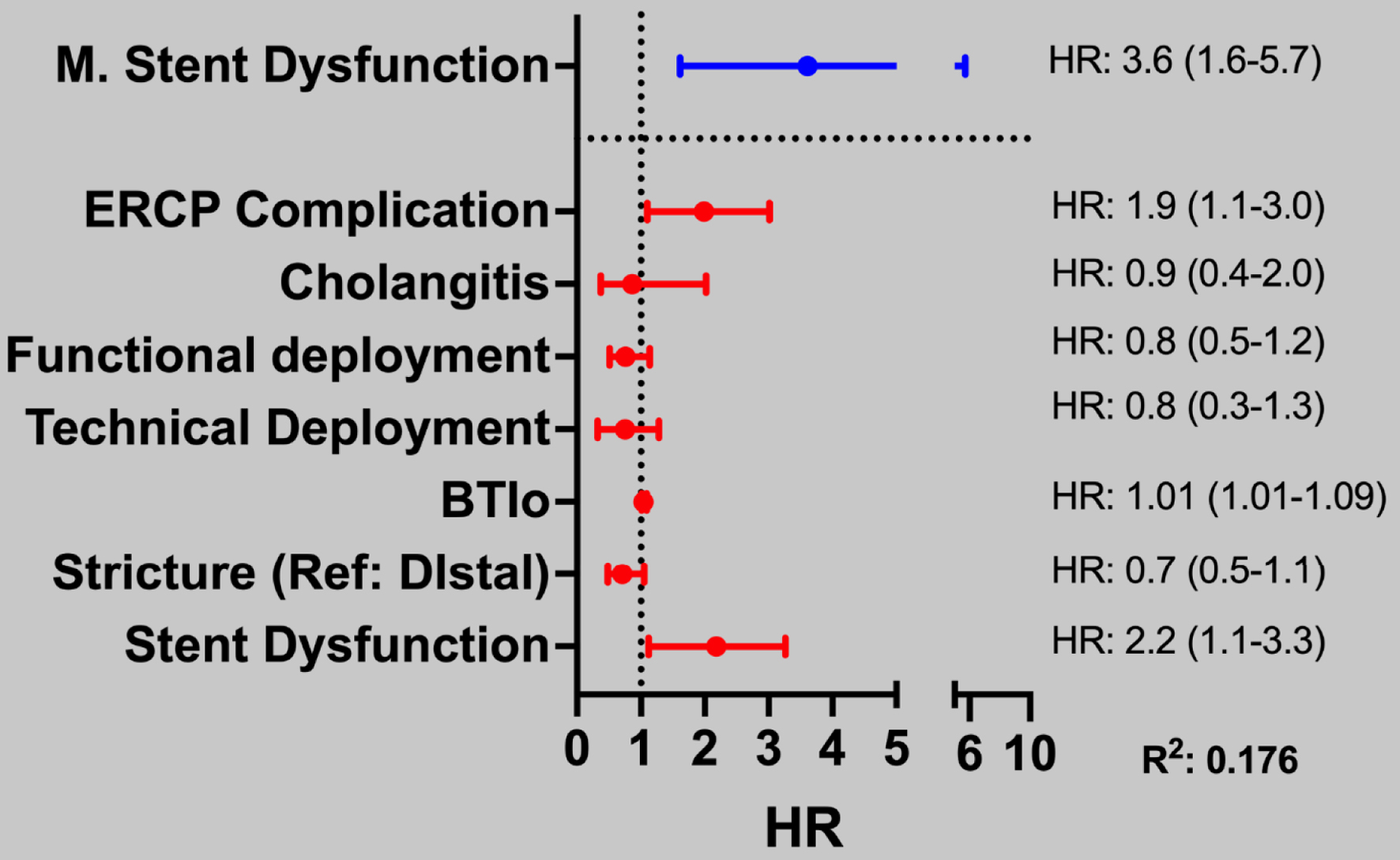
Figure 1. Multivariate Cox regression model for predicting variables associated with stent dysfunction in patients with malignant biliary stricture. Variables with statistical significance in the univariate model (represented in red) were applied in the multivariate model, which are represented in blue. For patients with malignant stenosis, the height of the distal stenosis is designated as the reference point. This distinction is vital for understanding the analyses and interpretations presented in the study, as it underscores the importance of comparing results across different statistical models. Such clarity enhances the reader’s ability to interpret the findings meaningfully and informs subsequent discussions on the implications of the data.