| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://gr.elmerpub.com |
Case Report
Volume 17, Number 5-6, December 2024, pages 217-223
Treatment of Crohn’s Disease With Infliximab and Subsequent Development of Takayasu’s Arteritis
Kei Nomuraa, Tomoyoshi Shibuyaa, b, c, Momoko Furushoa, Hirotaka Ishinoa, Masayuki Orikasaa, Masashi Omoria, Rina Odakuraa, Masao Komaa, Kentaro Itoa, Takafumi Maruyamaa, Dai Ishikawaa, b, Mariko Hojoa, b, Akihito Nagaharaa, b
aDepartment of Gastroenterology, Juntendo University School of Medicine, Bunkyo-ku, Tokyo 113-8421, Japan
bDepartment of Pathophysiological Research and Therapeutics for Gastrointestinal Disease, Juntendo University School of Medicine, Bunkyo-ku, Tokyo 113-8421, Japan
cCorresponding Author: Tomoyoshi Shibuya, Department of Gastroenterology, Juntendo University School of Medicine, Bunkyo-ku, Tokyo 113-8421, Japan
Manuscript submitted October 18, 2024, accepted November 23, 2024, published online December 28, 2024
Short title: TA Onset During IFX Treatment for CD
doi: https://doi.org/10.14740/gr1792
| Abstract | ▴Top |
A 23-year-old man was diagnosed with Crohn’s disease (CD) of the large intestine after colonoscopy revealed longitudinal ulcers, and pathology revealed non-caseating epithelioid cell granulomas and anal fistulas. The CD relapsed, and therefore prednisolone (PSL) and infliximab (IFX) treatment was initiated. The PSL was gradually tapered. Steroid-free remission was maintained with IFX. The patient subsequently developed a high fever and headache, while CD-related symptoms did not worsen. Laboratory data showed white blood cells at 14,200/µL and C-reactive protein at 17.2 mg/dL. Contrast-enhanced computed tomography revealed thoracoabdominal aortitis, and the patient was consequently diagnosed with Takayasu’s arteritis (TA). We therefore again initiated PSL treatment that immediately reduced the fever and headache. The PSL dose was again tapered and the administration of IFX was resumed to maintain CD remission. No further episodes of aortitis relapse were noted after restarting IFX, and the CD currently remains in remission. This is a rare case of TA onset during IFX treatment for CD, and, as such, contributes to the limited literature on such cases. More specifically, this case highlights that when patients with CD present with symptoms such as fever or headache, it is necessary to investigate the possibility of vasculitis.
Keywords: Crohn’s disease; Infliximab; Prednisolone; Takayasu’s arteritis
| Introduction | ▴Top |
Crohn’s disease (CD) is a chronic inflammatory disorder of the gastrointestinal tract, characterized by transmural inflammation with granulomatous alterations and longitudinal ulcers or skip lesions on endoscopy. CD is sometimes associated with extraintestinal complications, such as uveitis, arthritis, and erythema nodosum. Similarly, Takayasu’s arteritis (TA) is a rare granulomatous vasculitis that affects the aorta and its major vessels. These are chronic inflammatory diseases that are viewed as immunological disorders. However, the mechanisms involved in the pathogenesis of such diseases remain unknown.
Although the prevalence of both CD and TA is estimated to be 1 per 10 billion, cases involving the concurrent onset of these diseases have been reported [1-4]. Both are chronic inflammatory diseases of unknown cause that commonly occur in young people. It is likely that the pathogenesis of CD is related in some way to that of TA, although this phenomenon is not yet well understood.
Anti-tumor necrosis factor (TNF)-α agents are used to treat both TA and CD, although some patients with CD paradoxically develop TA during treatment with such drugs [5-18]. This paradoxical effect is thought to be caused by suppression of immune regulation due to TNF-α. Specifically, suppression of TNF-α may reduce T-cell regulatory function and increase the risk of autoimmune inflammation [19, 20]. We herein report the case of a 23-year-old man with CD who developed aortitis, consistent with the features of TA, despite receiving treatment with infliximab (IFX) for the CD.
| Case Report | ▴Top |
A 23-year-old man was diagnosed with CD of the large intestine after colonoscopy revealed longitudinal ulcers, and pathological findings revealed non-caseating epithelioid cell granulomas and anal fistulas. He presented to our department, and we continued the administration of mesalazine at a dose of 3 g/day. He was in remission for CD for 3 years. However, he experienced abdominal pain and diarrhea due to a relapse of CD. We therefore started treatment with prednisolone (PSL) and IFX at an initial dose of 5 mg/kg. After the induction of PSL and IFX therapy, the abdominal pain improved, and the frequency of defecation decreased. The PSL was gradually tapered, and steroid-free remission was maintained with IFX.
After 6 months, the patient presented with a high-grade fever and headache. Simultaneously, the serum C-reactive protein (CRP) level rose to 5.71 mg/dL, but influenza/coronavirus disease 2019 (COVID-19) tests were negative. Plain chest and abdominal computed tomography (CT) and head magnetic resonance imaging yielded no significant findings. The patient was referred to the Neurology Department of our hospital. However, signs of meningeal irritation were not observed, and a diagnosis of meningitis was negative. These symptoms and laboratory data are atypical of a CD relapse. Due to persistent spontaneous head pain and worsening fever, the patient was admitted to hospital for further investigation and treatment.
Other than the CD, the patient’s medical history was unremarkable. Physical examination revealed a height of 179 cm, weight of 53.6 kg, and body mass index of 16.7 kg/m2. The patient’s vital signs were stable (body temperature 40.2 °C; blood pressure 124/80 mm Hg and 120/74 mm Hg in right and left brachial arteries, respectively; heart rate 86 beats per minute (bpm), peripheral oxygen saturation (SpO2) 97% on room air). The patient complained of a headache with spontaneous pain throughout his head. No remarkable findings were noted in an abdominal examination. The frequency of defecation remained at approximately once daily, and no diarrhea was noted. Laboratory data revealed: white blood cells: 14,200/µL; hemoglobin, 13.3 g/dL; platelets, 57.5 × 104/µL; and CRP 17.2 mg/dL (Table 1). Various culture tests were performed but all were negative. A colonoscopy revealed ulcer scars throughout the large intestine, but the mucosa appeared to be in remission (Fig. 1). Small intestine capsule endoscopy revealed a normal small intestine mucosa, and, considering the absence of abdominal symptoms, the CD was determined to be in remission. Thoracoabdominal contrast-enhanced CT that was performed to investigate the source of a fever revealed wall thickening of the thoracoabdominal aorta and bilateral renal arteries, as well as focal stenosis at the origin of the right renal artery (Fig. 2). Positron emission tomography-CT showed abnormal accumulation around the celiac artery and para-aortic lymph nodes (Fig. 3). There was no obvious source of infection. We thus suspected that the patient had developed aortitis during the course of treatment for CD. TA was diagnosed based on the symptoms of fever, headache, and wall thickening and stenosis of the aorta. PSL 50 mg per day was started on the 17th day of illness for TA, and symptoms improved. PSL was effective and tapered down to the following schedule: 45 mg for 2 weeks, followed by 40 mg for 2 weeks. No recurrence of symptoms was observed. The patient was consequently discharged on the 59th day of hospitalization. PSL is being tapered off with treatment as an outpatient. At the time of writing, the patient had no signs of fever or complaints of diarrhea or abdominal pain, which suggested that the CD was in clinical remission.
 Click to view | Table 1. Laboratory Findings on Admission |
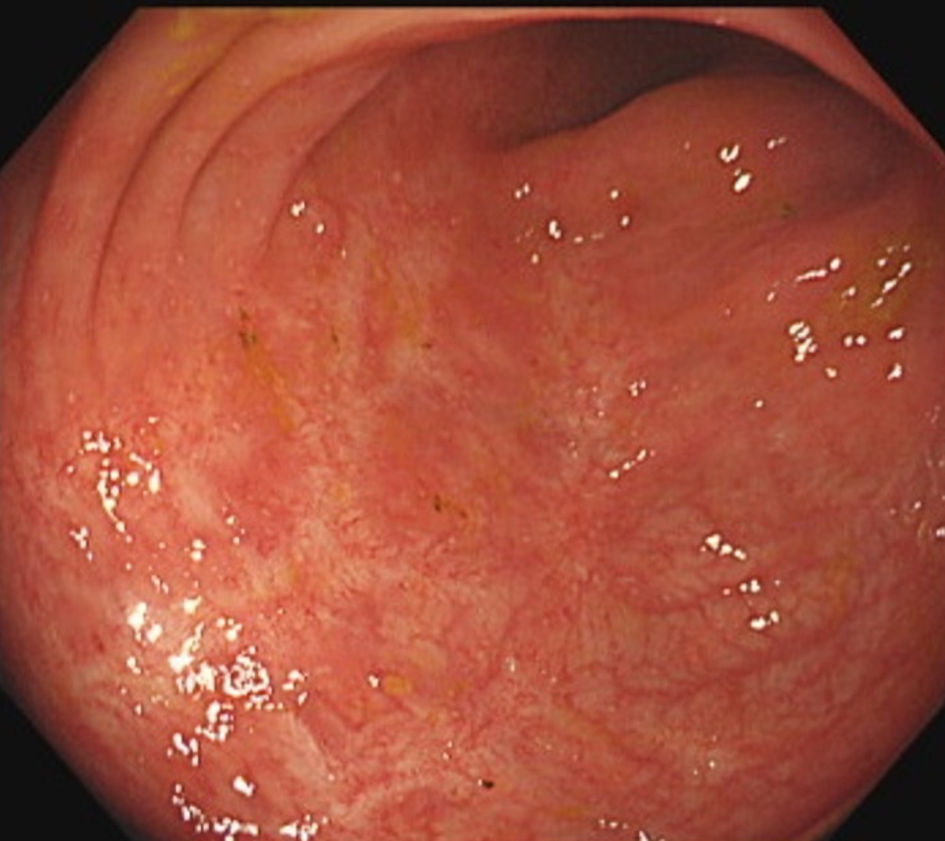 Click for large image | Figure 1. Colonoscopy revealed ulcer scars throughout the large intestine, but the mucosa appeared to be in remission. |
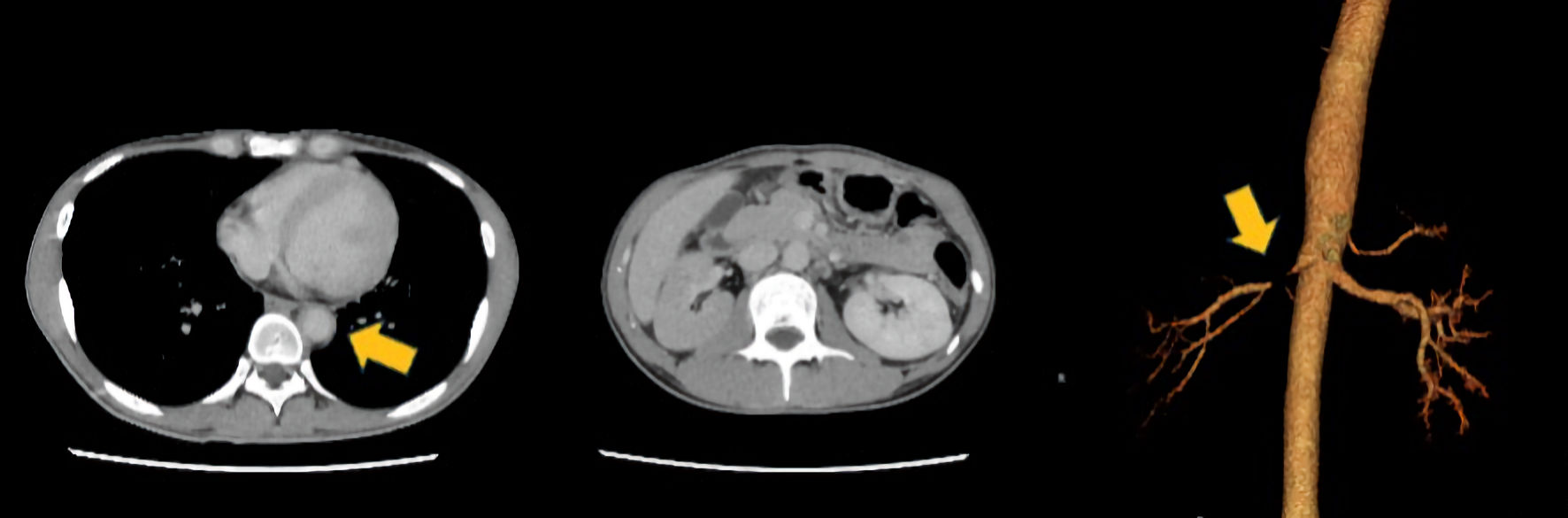 Click for large image | Figure 2. Computed tomography revealed wall thickening of the thoracoabdominal aorta and bilateral renal arteries (arrow in the left image) as well as focal stenosis (arrow in the right image) at the origin of the right renal artery. |
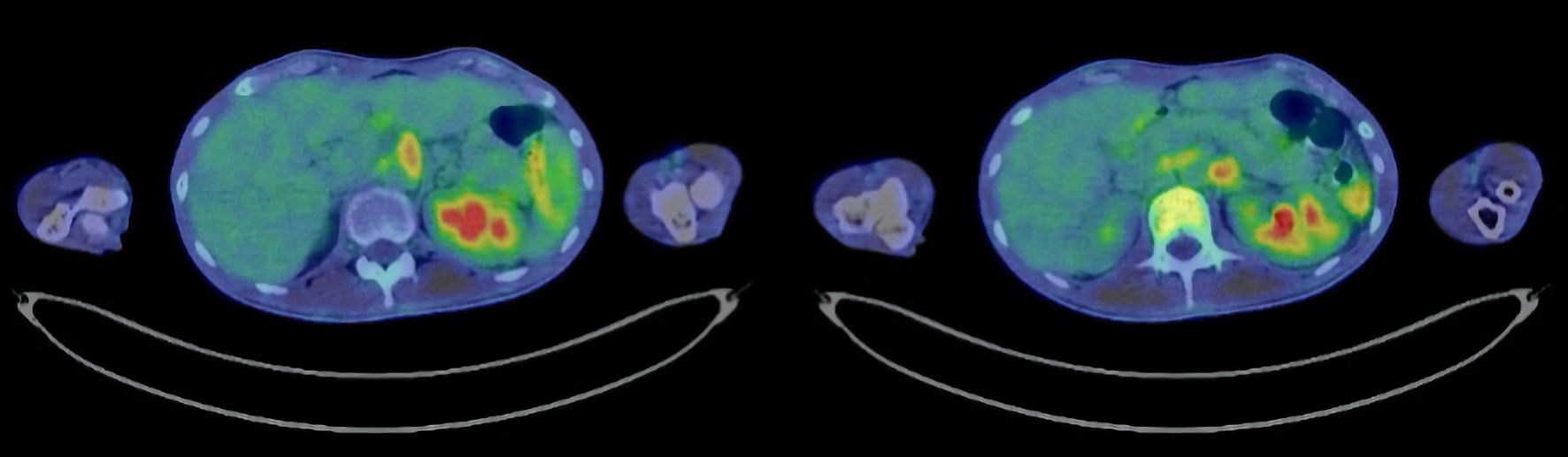 Click for large image | Figure 3. Positron emission tomography-computed tomography revealed abnormal accumulation around the celiac artery and para-aortic lymph nodes. |
| Discussion | ▴Top |
This is a rare case of CD where the patient developed aortitis with IFX treatment. IFX is used in the treatment of several autoimmune disorders, including TA; however, this case remains rare in terms of the development of aortitis while the patient was under IFX therapy. The frequency of defecation did not increase, and the patient did not complain of diarrhea. Hence, his symptoms, such as a high-grade fever and headache, differed from those observed at the beginning of the CD disease course, leading us to speculate that the inflammation was due to the associated aortitis. After starting the administration of PSL, the patient’s serum CRP level and fever quickly improved, indicating that the PSL was effective.
CD often exhibits extraintestinal complications, including uveitis, polyarthritis, primary sclerosing cholangitis, erythema nodosum, pyoderma gangrenosum, psoriasis, autoimmune thyroiditis, thromboembolism, and vasculitis. Arthritis is the most common extraintestinal complication, with 20% of patients with CD having some form of arthritis. However, the occurrence of vasculitis such as TA, particularly in large blood vessels, is a rare complication of CD. Nevertheless, several cases of CD that correlate with TA have been described [1-4].
TA is a nonspecific large-vessel vasculitis of unknown cause that leads to stenosis, occlusion, or dilated lesions in the aorta, its major branches, pulmonary arteries, and coronary arteries, and commonly occurs in young women. It is characterized by full-thickness arteritis. Based on the number of recipients of intractable disease benefits from the Ministry of Health, Labor and Welfare, the number of patients with TA in Japan is estimated to be approximately 5,000, with a male-to-female ratio of approximately 1:9. Although the mechanism of onset is unknown, it is speculated that some type of viral infection may be the trigger, leading to the destruction of vascular tissue by mainly T cells. As a known extraintestinal complication of inflammatory bowel disease, the association between TA and CD was first reported by Yassinger et al in 1976 [21]. The frequency of CD in TA is from 3.3% to 9.1%. Some kind of relationship is assumed between the comorbidity of both diseases [1, 22].
In the present case, the patient’s aortitis met some of the criteria for TA as defined in Japanese Circulation Society guidelines, including fever, increased acute-phase reactions and thickening of the thoracoabdominal aorta wall as shown by contrast-enhanced CT. According to the criteria of the American College of Rheumatology, one of six criteria, namely being < 40 years, must be met in association with the fulfillment of three or more items for a definition of TA [23-25]. These criteria include arteriogram abnormalities and occlusion or narrowing of the aorta or its major branches. The current case involved abnormal findings of narrowing and thickening of the aorta wall on CT. Based on such findings, the aortitis found could not be definitively diagnosed as TA but rather possible TA.
We conducted a literature review of CD and the use of TNF-α agents with TA. Medical databases were searched for relevant papers published after 2000, including in the Japan Medical Abstracts Society and PubMed. We found 17 previously reported cases [5-18] (Table 2). In a review of cases reported, the male-to-female ratio was 6:11, indicating slightly more prevalence of CD with TA in females. However, in cases of TA associated with CD, more awareness should be raised about the coexistence of TA in males with CD. A definitive diagnosis of TA is made by imaging of vascular lesions, such as stenosis and wall thickening, using angiography, digital sub-traction angiography, contrast-enhanced CT, and magnetic resonance angiography. As the disease progresses, patients begin to exhibit clinical symptoms based on ischemia. However, in the early stages, patients often have only nonspecific symptoms, such as fever and general malaise, and no specific blood test findings are apparent. Evidence of inflammatory reactions, such as increased erythrocyte sedimentation rate and CRP, and anemia, is said to be helpful in making a diagnosis. However, it is not easy to diagnose complications of TA during treatment for CD when clinical symptoms are mild. In our case, diarrhea and abdominal pain improved with IFX administration, and although scarring was observed in longitudinal ulcers throughout the large intestine, fever and elevated CRP levels were also observed. We should have suspected TA and performed a contrast-enhanced CT earlier at the first sign of a high fever. TA is generally said to respond well to steroids, and in our case, fever and CRP levels significantly improved when steroids were administered at the time of hospitalization.
 Click to view | Table 2. Review of the Literature on Takayasu’s Arteritis With Anti-Tumor Necrosis Factor-α Agents Associated With Crohn’s Disease |
The mechanism by which CD and TA coexist is not clear. However, a common feature is that they are caused by inflammation dominated by Th1 lymphocytes. In addition, inflammatory cytokines, such as TNF-α, interleukin (IL)-6, IL-8, IL-12, and IL-18, are associated with the pathology [26-28].
It is well-known that the use of anti-TNF-α antibody preparations has significantly altered treatment strategies for CD. Interestingly, several reports also exist highlighting the efficacy of anti-TNF-α antibody preparations in treating TA. Minami et al examined reported cases of inflammatory bowel disease complicated by TA treated with anti-TNF-α antibody preparations [29]. They found that these preparations were effective for both CD and TA. However, in their own case series, symptoms of TA did not improve with IFX administration, and a progression in vascular lesions, such as right renal artery stenosis, was apparent.
However, it has been pointed out that anti-TNF-α antibody preparations may pose a risk of inducing vasculitis, including TA. Fever and inflammatory responses resistant to IFX are speculated to be clinical symptoms of TA. Therefore, when using anti-TNF-α antibody preparations, the potential development of TA should be considered, and careful monitoring is warranted. Vasculitis is a rare side effect of treatment with anti-TNF-α agents. However, small-vessel lesions are more common. Ramos-Casals et al reported that 72% of patients who developed vasculitis during anti-TNF-α treatment had concomitant cutaneous lesions [20, 30]. Furthermore, anti-TNF-α agents may also result in paradoxical effects, such as the development of psoriatic skin lesions [31]. The causal mechanism of these paradoxical effects remains unclear; however, it may involve an imbalance of cytokines toward interferons, chemokines and probably IL-17 [20].
The disease activities of CD and aortitis were apparently independent of each other in this case. Therefore, it is unlikely that the aortitis was an extraintestinal manifestation of the CD. In addition, several types of paradoxical effects have been reported in addition to psoriatic lesions, including vasculitis and arthritis [31]. For these reasons, it is necessary to highlight the possibility that the vasculitis observed in this case was due to a paradoxical effect.
Another inflammatory bowel disease, ulcerative colitis, also occurs, although relatively rarely, in association with TA. Over 30 cases of concomitant ulcerative colitis and TA have been reported to date [22]. Another report demonstrated that 7% of patients with TA develop inflammatory bowel diseases, including CD or ulcerative colitis [32].
How to properly adjust the dose of PSL used in the treatment of CD is another important issue. As described above, PSL has no effect in maintaining CD in remission, and we should taper the dose of this drug at this point. However, TA is known to be exacerbated at a high rate when the dose of PSL is reduced. In such cases, immunomodulator therapy is recommended as concomitant treatment. It has been reported that 66-84% of patients with TA require immunosuppressive agents, such as azathioprine or methotrexate, in addition to corticosteroids [33]. If the patient’s aortitis worsens during the course of tapering PSL, we will consider the concomitant use of an immunomodulator and may be forced to apply PSL at the maintenance dose.
In conclusion, we herein report a case of CD, in which the patient developed aortitis indicative of TA that was diagnosed based on symptoms of fever and headache, despite receiving treatment with IFX. For patients with CD, even when presenting only with symptoms such as fever or headache, it is necessary to investigate the possibility of vasculitis, including in other regions of the body.
Acknowledgments
None to declare.
Financial Disclosure
This research received no external funding.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
The patient gave written informed consent for the possible publication of images with guaranteed anonymity.
Author Contributions
KN and TS designed the research. KN and MF collected data. KN wrote the manuscript. TS, HI, M. Orikasa, M. Omori, RO, MK, KI, TM, DI, and MH reviewed the manuscript. AN was responsible for the submission. All authors have read and agreed to the published version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Reny JL, Paul JF, Lefebvre C, Champion K, Emmerich J, Bletry O, Piette JC, et al. Association of Takayasu's arteritis and Crohn's disease. Results of a study on 44 Takayasu patients and review of the literature. Ann Med Interne (Paris). 2003;154(2):85-90.
pubmed - Farrant M, Mason JC, Wong NA, Longman RJ. Takayasu's arteritis following Crohn's disease in a young woman: any evidence for a common pathogenesis? World J Gastroenterol. 2008;14(25):4087-4090.
doi pubmed - Kusunoki R, Ishihara S, Sato M, Sumita Y, Mishima Y, Okada M, Tada Y, et al. Rare case of Takayasu's arteritis associated with Crohn's disease. Intern Med. 2011;50(15):1581-1585.
doi pubmed - Yilmaz N, Can M, Alibaz-Oner F, Direskeneli H. Clinically silent Crohn's disease in a patient with Takayasu's arteritis unresponsive to conventional therapies. Rheumatol Int. 2013;33(12):3091-3093.
doi pubmed - Domenech E, Garcia-Planella E, Olazabal A, Sanchez-Delgado J, Zabana Y, Bernal I, Manosa M, et al. Abdominal aortitis associated with Crohn's disease. Dig Dis Sci. 2005;50(6):1122-1123.
doi pubmed - Kellermayer R, Jain AK, Ferry G, Deguzman MM, Guillerman RP. Clinical challenges and images in GI. Aortitis as a rare complication of Crohn's disease. Gastroenterology. 2008;134(3):668-898.
doi pubmed - El-Matary W, Persad R. Takayasu's aortitis and infliximab. J Pediatr. 2009;155(1):151.
doi pubmed - Katoh N, Kubota M, Shimojima Y, Ishii W, Matsuda M, Akamatsu T, Ikeda S. Takayasu's arteritis in a patient with Crohn's disease: an unexpected association during infliximab therapy. Intern Med. 2010;49(2):179-182.
doi pubmed - Okada H, Kurasawa K, Nomura Y, Onishi S, Arai S, Owada T, Maezawa R, et al. A case of Takayasu arteritis that developed during infliximab therapy for Crohn's disease. Proceedings of Kanto Rheumatology Conference. 2010;43:102-110. (in Japanese)
- Osman M, Aaron S, Noga M, Yacyshyn E. Takayasu's arteritis progression on anti-TNF biologics: a case series. Clin Rheumatol. 2011;30(5):703-706.
doi pubmed - Kiyohara H, Hisamatsu T, Matsuoka K, Naganuma M, Kameda H, Seta N, Takeuchi T, et al. Crohn's Disease in which the patient developed aortitis during treatment with adalimumab. Intern Med. 2015;54(14):1725-1732.
doi pubmed - Sy A, Khalidi N, Dehghan N, Barra L, Carette S, Cuthbertson D, Hoffman GS, et al. Vasculitis in patients with inflammatory bowel diseases: A study of 32 patients and systematic review of the literature. Semin Arthritis Rheum. 2016;45(4):475-482.
doi pubmed - Miyakawa M, Tanaka H, Yamashita M, Sakemi R, Nasuno M, Ishii M, Yanagisawa H, et al. [A case of Takayasu's arteritis detected in a patient with Crohn's disease following infliximab treatment]. Nihon Shokakibyo Gakkai Zasshi. 2016;113(10):1761-1768.
doi pubmed - Takeuchi I, Kawai T, Nambu M, Migita O, Yoshimura S, Nishimura K, Yoshioka T, et al. X-linked inhibitor of apoptosis protein deficiency complicated with Crohn's disease-like enterocolitis and Takayasu arteritis: A case report. Clin Immunol. 2020;217:108495.
doi pubmed - Kollen L, Werner O, Gavotto A. Uncommon cause of chest pain in a 9-year-old boy with Crohn's disease. Gastroenterology. 2020;158(8):2055-2057.
doi pubmed - Kishimoto K, Nozaki Y, Sakurai T, Kinoshita K, Funauchi M, Matsumura I. Takayasu's Arteritis Diagnosed in an Adolescent Patient with Crohn's Disease: Management of Biologicals. Life (Basel). 2021;11(10):1019.
doi pubmed - Fotis L, Kourti A, Prountzos S, Alexopoulou E, Papaevangelou V, Fessatou S. Takayasu arteritis in an adolescent with Crohn's disease. Rheumatol Int. 2022;42(3):563-570.
doi pubmed - Ariga H, Chino Y, Ojima T, Suzuki S, Okada K, Kashimura J. Takayasu's arteritis associated with Crohn's disease treated with infliximab. Clin J Gastroenterol. 2024;17(2):281-285.
doi pubmed - Tracey D, Klareskog L, Sasso EH, Salfeld JG, Tak PP. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. 2008;117(2):244-279.
doi pubmed - Wendling D, Prati C. Paradoxical effects of anti-TNF-alpha agents in inflammatory diseases. Expert Rev Clin Immunol. 2014;10(1):159-169.
doi pubmed - Yassinger S, Adelman R, Cantor D, Halsted CH, Bolt RJ. Association of inflammatory bowel disease and large vascular lesions. Gastroenterology. 1976;71(5):844-846.
pubmed - Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, Hoffman GS. Takayasu arteritis. Ann Intern Med. 1994;120(11):919-929.
doi pubmed - Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, Fauci AS, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990;33(8):1129-1134.
doi pubmed - de Souza AW, de Carvalho JF. Diagnostic and classification criteria of Takayasu arteritis. J Autoimmun. 2014;48-49:79-83.
doi pubmed - Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65(1):1-11.
doi pubmed - Maksimowicz-McKinnon K, Hoffman GS. Crohn's disease plus Takayasu's arteritis: more than coincidence? Ann Med Interne (Paris). 2003;154(2):75-76.
pubmed - Seko Y. Giant cell and Takayasu arteritis. Curr Opin Rheumatol. 2007;19(1):39-43.
doi pubmed - Pallone F, Monteleone G. Mechanisms of tissue damage in inflammatory bowel disease. Curr Opin Gastroenterol. 2001;17(4):307-312.
doi pubmed - Minami N, Nakase H, Yoshino T, Yamada S, Toyonaga T, Honzawa Y, Matsuura M, et al. Effect of infliximab on inflammatory bowel disease with Takayasu arteritis: case series and review of the literature. Clin J Gastroenterol. 2013;6(3):226-230.
doi pubmed - Ramos-Casals M, Brito-Zeron P, Cuadrado MJ, Khamashta MA. Vasculitis induced by tumor necrosis factor-targeted therapies. Curr Rheumatol Rep. 2008;10(6):442-448.
doi pubmed - Ramos-Casals M, Brito-Zeron P, Munoz S, Soria N, Galiana D, Bertolaccini L, Cuadrado MJ, et al. Autoimmune diseases induced by TNF-targeted therapies: analysis of 233 cases. Medicine (Baltimore). 2007;86(4):242-251.
doi pubmed - Ohta Y, Ohya Y, Fujii K, Tsuchihashi T, Sato K, Abe I, Iida M. Inflammatory diseases associated with Takayasu's arteritis. Angiology. 2003;54(3):339-344.
doi pubmed - Chatterjee S, Flamm SD, Tan CD, Rodriguez ER. Clinical diagnosis and management of large vessel vasculitis: Takayasu arteritis. Curr Cardiol Rep. 2014;16(7):499.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.