| Gastroenterology Research, ISSN 1918-2805 print, 1918-2813 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Gastroenterol Res and Elmer Press Inc |
| Journal website https://gr.elmerpub.com |
Original Article
Volume 000, Number 000, June 2025, pages 000-000
Endoscopic Biliary Drainage in Malignant Biliary Strictures: A Prospective Analysis Based on Real-World Data
Julio Zuniga Cisnerosa, b, e , Alexis Mc-Kenziec, Ivan Ramosc, Eric Ortizc, Orlando Quirosc, Calixto Duarte-Changd, Carlos Tunona
aDepartment of Gastroenterology, Instituto Oncologico de Panama, Panama City, Panama
bSchool of Medicine, University of Panama, Panama, Panama City, Panama
cDepartment of Gastroenterology, Complejo Hospitalario Metropolitano de Panama, Panama City, Panama
dDepartment of Gastroenterology, Hospital San Miguel Arcangel, Panama City, Panama
eCorresponding Author: Julio Zuniga Cisneros, Department of Gastroenterology, Instituto Oncologico de Panama, Panama City, Panama
Manuscript submitted April 28, 2025, accepted June 2, 2025, published online June 16, 2025
Short title: Endoscopic Drainage in MBS
doi: https://doi.org/10.14740/gr2046
| Abstract | ▴Top |
Background: Endoscopic biliary drainage has emerged as the standard treatment for palliative drainage in malignant biliary strictures (MBS).
Methods: This prospective study aimed to investigate the outcomes of patients diagnosed with MBS who underwent biliary drainage through endoscopic retrograde cholangiopancreatography (ERCP) at Complejo Hospitalario Metropolitano. The primary goals were to evaluate the stent dysfunction (SD) and mortality over a 12-month follow-up period. We evaluated the technical and functional deployment success rates according to the stricture location and type of stent used.
Results: Out of 191 patients screened, 147 were eligible for inclusion. Distal strictures exhibited significantly higher technical (96.3%) and functional (75.8%) success deployment rates compared to hilar strictures (32.4% technical, 58.8% functional). The overall incidence of SD reached 46.9%, while mortality was 43.5%. Notably, complications varied by stricture type, with bacteremia predominating in hilar stricture cases.
Conclusion: The findings from our prospective study affirm a commendably high rate of successful endoscopic stenting interventions along with a lower incidence of adverse events in patients suffering from MBS. Conversely, it is imperative to acknowledge that the endoscopic management of malignant hilar strictures necessitates a more individualized approach due to the elevated complication rates and increased likelihood of SD observed in our study.
Keywords: Endoscopic stenting; Malignant; Biliary stricture; Cholangiocarcinoma
| Introduction | ▴Top |
Endoscopic biliary drainage has emerged as the standard treatment for palliative drainage in malignant biliary strictures (MBS) [1, 2]. These strictures pose significant challenges in gastroenterology and oncology, necessitating a multidisciplinary approach for effective management. They can occur in both hilar and distal locations within the biliary tree, each presenting distinct treatment considerations [3].
Hilar strictures, located near the liver hilum, often require advanced endoscopic techniques or percutaneous interventions due to their proximity to critical vascular and biliary structures [4-8]. In contrast, distal strictures, situated closer to the duodenum, may be more amenable to interventions such as endoscopic retrograde cholangiopancreatography (ERCP) with stent placement or even surgical resection. Regardless of stricture location, successful endoscopic drainage is associated with reduced mortality and lower complication rates [3, 9-12].
Two types of stents are typically used for effective endoscopic biliary drainage: plastic stents (PS) and self-expanding metal stents (SEMS). Each type exhibits unique characteristics related to stent patency, the need for reintervention, potential dysfunction, and adverse events [10, 13-16]. Although SEMS are increasingly favored for their prolonged patency, evidence supports their use primarily in distal strictures. The data in proximal strictures remain inconsistent, indicating a need for additional prospective studies [9, 12, 17-19].
The objective of this research was to evaluate the endoscopic stenting for MBS, comparing outcomes based on the stricture location (hilar versus distal). A prospective analysis was conducted to assess the 12-month rates of stent dysfunction (SD), ERCP complications, and mortality at a third-level hospital in Central America.
| Materials and Methods | ▴Top |
Study design
This was a prospective study that included all patients diagnosed with MBS who were referred to the Gastrointestinal Department at Complejo Hospitalario Metropolitano and underwent biliary drainage using ERCP between June 2021 and June 2023. The study received approval from the Hospital’s Bioethics committee. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
We conducted a 12-month follow-up on patients who underwent ERCP. During this period, we recorded events such as SD, ERCP complications, the date of histological diagnosis, and mortality rates.
All participants enrolled in this study should have a verified diagnosis of malignant disease. The diagnosis of MBS was confirmed through histopathological analysis of samples obtained via multiple procedures, including ERCP, endoscopic ultrasound (EUS), computed tomography (CT)-guided biopsy, endoscopy, and surgical intervention. If histology could not be obtained or if it yielded inconclusive results, a strong suspicion based on the patient’s clinical presentation, CT scans, and ERCP findings was also taken into account.
We excluded patients who were under the age of 18, patients who were suitable for percutaneous biliary drainage as the initial choice, and patients who had previously received a biliary stent. The patients were categorized into two groups based on the indication for stenting: distal stricture, which was situated below the junction of the cystic duct and biliary duct, and hilar stricture, which was located above this junction. Patients with Bismuth-Corlette (BC) I stricture were classified as lower stricture.
Technical deployment of biliary stent
The ERCP procedures were conducted by highly skilled endoscopists, each with a track record of doing over 1,500 procedures. The Pentax video duodenoscope ED34-i10T2 series was used for these procedures.
The decision between a unilateral or bilateral drainage stent was determined by the indication of biliary drainage following American Society of Gastrointestinal Endoscopy (ASGE) guidelines [1], technical aspects of the procedure, and the availability of medical supplies for performing complex procedures. An uncovered self-expandable metal stent (uSEMS) was exclusively implanted in individuals who had histologically proven malignancy and had been determined surgically irresectable. We exclusively utilized Wallstent uSEMS manufactured by Boston Scientific in Galway, Ireland.
Study variables and definitions
Technical success was defined as a successful deployment of a PS or SEMS positioned 2 cm above the narrowing of the bile duct, allowing for drainage of at least > 50% of the liver volume including the lobe with the most significant enlargement shown on previous imaging. Functional success was defined as a reduction in bilirubin levels by over 50% compared to the initial value, more than 14 days after stent placement [20]. The resectability of pancreatic cancer was determined based on the MD Anderson criteria, which relied on CT findings [21]. The determination of the Bismuth type was made via direct cholangiography. ERCP complications were characterized during the first 7 days following the procedure and included post-ERCP pancreatitis, post sphincterotomy hemorrhage (a drop of 2 g/dL hemoglobin), sepsis or bacteremia after ERCP, and intestinal perforation.
SD was diagnosed according to the criteria proposed by Scmidt et al [13] which include biliary dilatation observed on ultrasound (compared to the bile duct diameter measured after stenting), bilirubin concentration equal to or greater than 2 mg/dL or a difference of more than 1 mg/dL (compared to the previous value recorded after successful stenting), an increase in gamma-glutamyl transpeptidase (GGT) or alkaline phosphatase (ALP) exceeding twice the normal value, and symptoms indicative of cholangitis such as fever, leukocyte count greater than 10,000, and increased C-reactive protein (CRP) levels.
Mortality was documented if it happened after 12 months of monitoring following the first ERCP performed.
To prevent post-ERCP pancreatitis, patients were given appropriate intravenous hydration at a dosage of 20 mL/kg bolus periprocedure. Antibiotic prophylaxis was administered in accordance with the guidelines published by the European Society of Gastrointestinal Endoscopy (ESGE) [22].
Statistical analysis
The statistical analysis was conducted using Stata/SE 16.0 software (Stata Corp., College Station, TX, USA). We conducted a Kolmogorov-Smirnov test to assess the normal distribution of continuous data. Our data did not follow a normal distribution.
The data for continuous variables were represented using the median in addition to the interquartile range (IQR). Quantitative variables were represented numerically as percentages. The Mann-Whitney test was employed to analyze continuous variables that were not paired, whereas the Chi-squared test was utilized to assess differences among qualitative variables. For paired quantitative variables (e.g. bilirubin), we used Wilcoxon-paired test. The results were deemed statistically significant with a P-value of less than 0.05 (two-tailed).
We conducted two models using Cox multivariate regression analysis. The first model oriented to find factors related with biliary SD and the second model to find associated factors with mortality. The model’s quality was assessed using Cox and Snell’s R2 and Nagelkerke test. The Cox regression coefficients were transformed into odds ratios (ORs) and their corresponding 95% confidence intervals (CIs) using conventional techniques.
A Kaplan-Meier curves and log rank test were employed to compare differences in cumulative event for SD or mortality in patients with MBS by type of stricture and type of stent (PS or uncovered SEMS) employed in high and lower MBS.
| Results | ▴Top |
We identified 191 patients who fulfilled inclusion criteria during the time of the study. Of those patients, we excluded 15 patients with indeterminate stricture and 29 patients with failure to perform ERCP. A total of 147 patients were included in the study. Patients with MBS had a median age of 70.5 years (IQR 60 - 78) and 53.1% were females. In our study, pancreatic cancer and cholangiocarcinoma were the most frequent malignancies in distal strictures (58.7%) and hilar strictures (36.9%), respectively.
Bilirubin levels in patients with hilar and distal stricture were 15.2 mg/dL (IQR: 10.2 - 22.4) and 17.5 mg/dL (IQR: 12 - 23.1) (P = 0.686), respectively.
Patients undergoing hilar stenting had a successful technical drainage of 32.4% and a functional drainage of 58.8%. In comparison, patients undergoing stenting of distal stricture had a successful technical drainage of 96.3% and functional drainage of 75.8%. During the 12-month follow-up time, 46.9% patients had SD and 43.5% patients died (Table 1).
 Click to view | Table 1. Characteristic of Patients With Malignant Biliary Stenosis Based on Location of the Malignant Biliary Stricture |
In patients with hilar stricture, 92.1% had PS deployment and 7.9% had uSEMS deployment. In contrast, in patients with distal stricture, 88% had PS deployment and 12% had uSEMS, with no statistical differences. Regarding ERCP complications, bacteremia (22.8%) was the most common complication in patients with hilar strictures and bleeding (5.2%) and pancreatitis (5.2%) were the most frequent complications in patients with distal stricture (Table 2).
 Click to view | Table 2. Characteristic of Patients With Biliary Malignant Strictures According to Stricture Location and Type of Stent |
SD was more common in patients with PS and hilar stricture (66.6%) than uSEMS (33.2%) (P = 0.146). In patients with distal stricture with uSEMS, 38.4% and 42.6% with PS had SD (Table 2).
Predicting SD and mortality
In Figure 1, the multivariate Cox regression model for predicting SD shows that ERCP complications (hazard ratio (HR): 5.2, 95% CI: 1.3 - 9.1), cholangitis (HR: 2.3, 95% CI: 1.1 - 3.8), and proximal stricture (HR: 2.3, 95% CI: 1.4 - 4.1) were the only variables associated with SD. In Figure 2, a multivariate Cox regression model for predicting mortality, after adjusting evidence, shows that only SD was associated with mortality (HR: 3.6, 95% CI: 1.6 - 5.7).
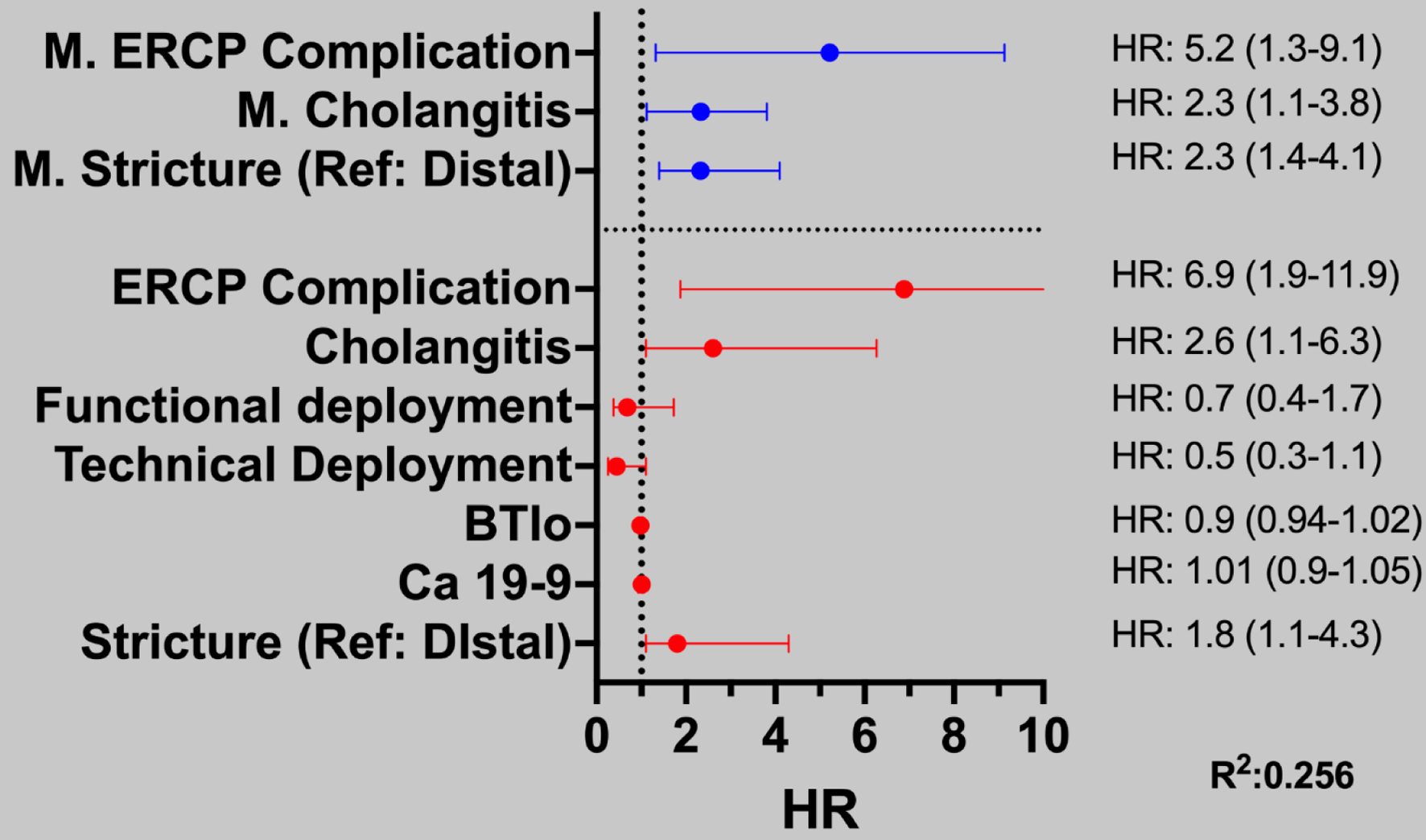 Click for large image | Figure 1. Multivariate Cox regression model for predicting variables associated with stent dysfunction in patients with malignant biliary stricture. Variables with statistical significance in the univariate model (represented in red) were applied in the multivariate model, which are represented in blue. For patients with malignant stenosis, the height of the distal stenosis is designated as the reference point. This distinction is vital for understanding the analyses and interpretations presented in the study, as it underscores the importance of comparing results across different statistical models. Such clarity enhances the reader’s ability to interpret the findings meaningfully and informs subsequent discussions on the implications of the data. |
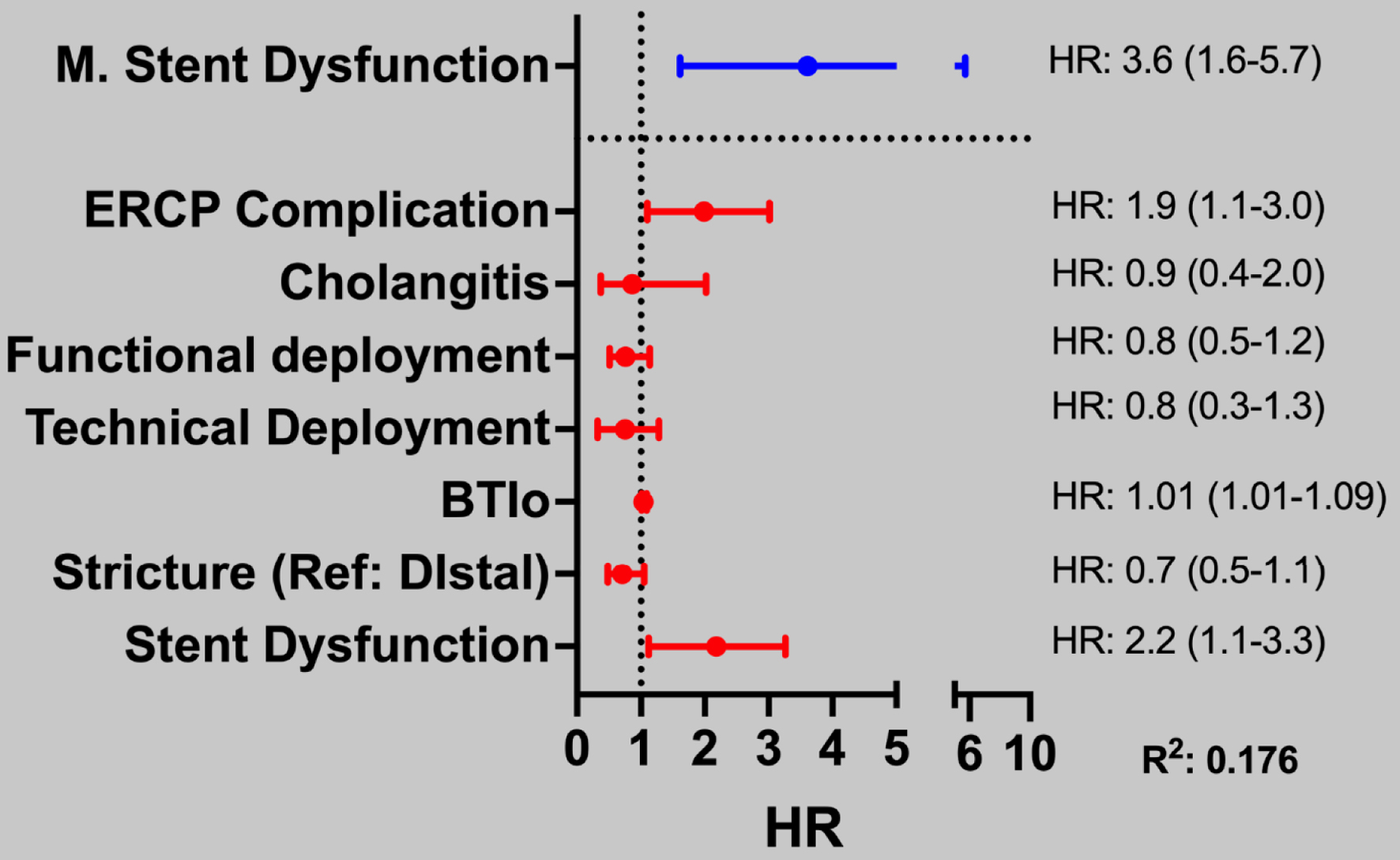 Click for large image | Figure 2. Multivariate Cox regression model for predicting variables associated with mortality in patients with malignant biliary stricture. Variables with statistical significance in the univariate model (represented in red) were applied in the multivariate model, which are represented in blue. For patients with malignant stenosis, the height of the distal stenosis is designated as the reference point. This distinction is vital for understanding the analyses and interpretations presented in the study, as it underscores the importance of comparing results across different statistical models. Such clarity enhances the reader’s ability to interpret the findings meaningfully and informs subsequent discussions on the implications of the data. |
Cumulative event and survival analysis based on type of stent and stricture location
Figure 3 shows the cumulative event for combined outcome of mortality/SD after stent placement. In patients with distal stricture, there was an 86% increased risk of SD/mortality between distal PS and distal uSEMS (HR: 1.86, 95% CI: 0.98 - 3.51, P = 0.056), showing no statistically significant differences. There was no difference between hilar uSEMS vs. hilar PS (HR: 1.30 (0.73 - 2.32), P = 0.380).
 Click for large image | Figure 3. Cumulative event for stent dysfunction or mortality in patients with malignant biliary stricture by type of stricture and type of stent. |
Figure 4 show a survival analysis after stent placement by location of the stricture (distal and hilar). In patients with distal stricture, there was a reduced risk of 22% mortality with distal uSEMS vs. distal-PS (HR: 0.78 (0.63 - 0.94), P = 0.021). There were no statistical differences in hilar strictures (P = 0.439).
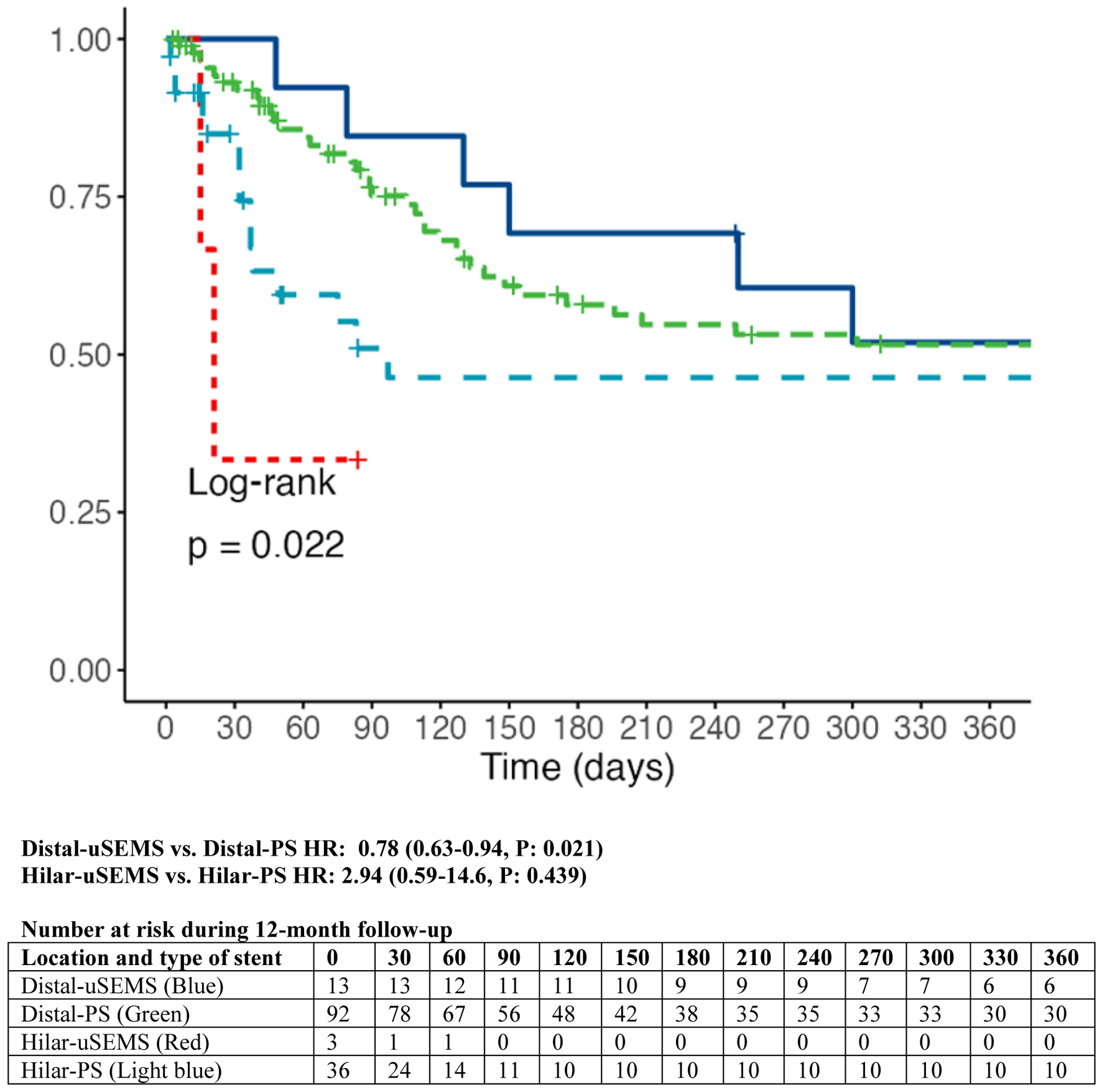 Click for large image | Figure 4. Survival analysis in patients with malignant biliary strictures according to location of the stricture and type of stent. |
| Discussion | ▴Top |
Our study represents a significant contribution to the field as it is the first report in Panama and Central America to investigate the outcomes of mortality and SD in patients with MBS following stenting over a 12-month period. We specifically focused on comparing outcomes based on the type of stent used, uSEMS versus PS, and the anatomical location of the stricture. Our findings revealed that in cases of distal strictures, uSEMS demonstrated remarkably lower rates of SD, mortality, and complications associated with ERCP. Conversely, patients with hilar strictures experienced a higher incidence of ERCP-related complications and a significantly increased risk of SD with plastic and uSEMS.
Numerous prospective analyses and clinical trials have consistently affirmed the superiority of SEMS over PS in providing effective palliative drainage of the biliary tract [13, 14]. However, our study revealed a lower functional success rate in managing distal stenosis compared to earlier reports [3, 10, 14, 17]. This disparity may be partly attributable to the elevated bilirubin levels observed in our patient cohort, as well as a lower application rate of uSEMS in our practice. Furthermore, existing literature indicates that pre-stenting bilirubin levels above 10 mg/dL are significantly associated with a delayed rate of bilirubin normalization, thereby underscoring the importance of careful patient selection and stent choice based on clinical presentation [23].
Our analysis yielded a mean patency duration of 249 days for uSEMS compared to 86 days for PS, with corresponding SD rates of 49.5% and 38.4% after 12 months, which emphasizes the advantages of using uSEMS in enhancing patency and minimizing complications. Prospective studies and clinical trials have robustly demonstrated that uSEMS achieve a mean patency duration of approximately 250 days, whereas PS typically exhibits patency lasting 50 to 66 days; these findings are consistently reinforced by clinical studies concerning distal stenosis [10, 14, 17]. In patients with unresectable tumors who qualify for palliative drainage, uSEMS reveal markedly superior patency rates coupled with significantly lower complication rates (7.7% compared to 24.8%) [1, 3, 13, 17]. Notably, we did not have reported cases of bleeding associated with uSEMS, highlighting their safety profile. Collectively, these outcomes not only emphasize the benefits of utilizing SEMS but also resonate with findings from existing research advocating for their preferential use in clinical practice in the appropriate clinical context. Conversely, hilar stent patency rates were less favorable, with 24 days for PS and 84 days for uSEMS, showing no statistically significant differences. This finding highlights the inherent challenges and complexities of managing hilar strictures, which often necessitate a tailored approach depending on the clinician’s expertise and the available medical resources.
Overall, the incidence of SD was notably higher in proximal stents when compared to distal stents, recorded at 60.5% versus 42% (P = 0.001). However, the literature concerning stent patency presents a context of contradiction; while some studies advocate for the advantages of metal stent placements, others fail to demonstrate significant differences in outcomes between partially covered SEMS and uSEMS [2, 3, 9, 24]. This disparity in findings underscores the need for further investigation to clarify the optimal stent choice in various clinical scenarios.
Our research also sheds light on the difficulties encountered in managing biliary strictures, particularly among patients with advanced cholangiocarcinoma. We incorporated patients diagnosed with cholangiocarcinoma classified as BC type I as distal strictures, reasoning that their behavior is similar to that of distal strictures, and also with around 50% of our sample fitting this definition. For hilar strictures, we observed a technical deployment success rate of 34.2% and a functional success rate of 63.2%, which aligns with findings from other prospective studies, despite variability in the definition of functional drainage across research works [2, 9, 12, 17, 18, 24]. Notably, 28.9% of hilar stenosis cases could not achieve an appropriate technical stent deployment by definition; nonetheless, we successfully attained functional drainage in these patients. We believe our results may have been influenced by the significant proportion of patients with BC type III and IV cholangiocarcinoma, conditions that complicate the drainage strategy and underscore the necessity of considering a mixed approach that may incorporate both percutaneous and EUS drainage techniques. In our clinical experience, managing hilar strictures proved particularly challenging, especially in cases of BC type III and IV cholangiocarcinomas. The selection of an appropriate biliary drainage method and stent type often hinges on the clinician’s technical expertise and the availability of specialized resources. While the use of metal stents in higher strictures lacks robust evidence, various studies produce conflicting results, suggesting an ongoing debate within the medical community regarding the best practices in this area [9, 12, 17-19, 24]. The selection of an optimal drainage strategy and stent type is paramount and may shift in response to emerging trends in chemotherapy and immunotherapy, which could significantly change the landscape of treatment for these patients.
Moreover, the study observed that post-procedural adverse events, notably bacteremia, were more prevalent in the context of hilar stenting compared to distal stenting. This finding is consistent with the technical challenges faced when attempting to achieve appropriate liver drainage in these cases [25, 26]. Thus, we recommend adopting a stepwise, multidisciplinary approach that incorporates ERCP, ultrasound, and interventional radiology techniques to secure functional drainage for patients presenting with intrahepatic hilar strictures. Identifying specific variables linked to SD, such as complications during ERCP and instances of cholangitis, allows for potential early intervention, aiming to improve patient outcomes. Our data underlined the significant association between SD and mortality risk, advocating for strategies focused on ensuring functional drainage and expeditious stent replacement to improve survival rates.
This study provides critical insights into the real-world outcomes of stenting for MBS, operating outside the confines of controlled clinical trial environments. An important limitation of our study was the restricted ability to utilize magnetic resonance imaging for planning the ERCP intervention. This constraint stemmed from the considerable challenges posed by the lengthy waiting times for magnetic resonance imaging, making it impractical in a clinical context. Consequently, we frequently opted to perform ERCP based on CT scan results. Although this choice may have affected our final outcomes, it effectively reflects the realities encountered in a tertiary hospital where there is a high demand for ERCP services amidst limited resources. While we recognize the limitations of our analysis, such as the exclusion of patients treated with percutaneous stents and the limited availability of particular stent types, we strongly advocate for further prospective and multicenter research endeavors. Such studies are essential to refine and enhance the management of biliary strictures, especially in the evolving context of treatment modalities, including immunotherapy approaches. Our findings are a call to action for clinicians and researchers alike to prioritize individualized patient care strategies that aim to optimize outcomes in this challenging patient population.
In conclusion, the findings from our prospective studies affirm a commendably high rate of successful endoscopic stenting interventions along with a lower incidence of adverse events in patients suffering from malignant distal biliary strictures treated with uSEMS. Conversely, it is imperative to acknowledge that the endoscopic management of malignant hilar strictures necessitates a more individualized approach due to the elevated complication rates and increased likelihood of SD observed in our study.
Acknowledgments
Thanks to the personnel of Radiology and Gastroenterology Department at Complejo Hospitalario Metropolitano.
Financial Disclosure
This study did not receive any financial support from governmental institutions or private companies.
Conflict of Interest
The authors have no potential conflict of interest.
Informed Consent
Every patient provided their informed consent prior to undergoing the procedure.
Author Contributions
JZC: conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing-original draft, and writing-review and editing. AMcK: investigation, methodology, project administration, resources, validation, writing-original draft, and writing-review and editing. IR, EO, and CDC: investigation, methodology, resources, validation, writing-original draft, and writing-review and editing. OQ and CT: investigation, methodology, validation, writing-original draft, and writing-review and editing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Qumseya BJ, Jamil LH, Elmunzer BJ, Riaz A, Ceppa EP, Thosani NC, Buxbaum JL, et al. ASGE guideline on the role of endoscopy in the management of malignant hilar obstruction. Gastrointest Endosc. 2021;94(2):222-234.e222.
doi pubmed - Elmunzer BJ, Maranki JL, Gomez V, Tavakkoli A, Sauer BG, Limketkai BN, Brennan EA, et al. ACG clinical guideline: diagnosis and management of biliary strictures. Am J Gastroenterol. 2023;118(3):405-426.
doi pubmed - Lubbe J, Sandblom G, Arnelo U, Jonas E, Enochsson L. Endoscopic stenting for malignant biliary obstruction: results of a nationwide experience. Clin Endosc. 2021;54(5):713-721.
doi pubmed - Lee TH, Moon JH, Park SH. Biliary stenting for hilar malignant biliary obstruction. Dig Endosc. 2020;32(2):275-286.
doi pubmed - Afshar M, Khanom K, Ma YT, Punia P. Biliary stenting in advanced malignancy: an analysis of predictive factors for survival. Cancer Manag Res. 2014;6:475-479.
doi pubmed - Fernandez YVM, Arvanitakis M. Early diagnosis and management of malignant distal biliary obstruction: a review on current recommendations and guidelines. Clin Exp Gastroenterol. 2019;12:415-432.
doi pubmed - Dumonceau JM, Tringali A, Papanikolaou IS, Blero D, Mangiavillano B, Schmidt A, Vanbiervliet G, et al. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy. 2018;50(9):910-930.
doi pubmed - Domper Arnal MJ, Simon Marco MA. Endoscopic management of malignant biliary stenosis. Update and highlights for standard clinical practice. Rev Esp Enferm Dig. 2016;108(9):568-575.
doi pubmed - Cassani LS, Chouhan J, Chan C, Lanke G, Chen HC, Wang X, Weston B, et al. Biliary decompression in perihilar cholangiocarcinoma improves survival: a single-center retrospective analysis. Dig Dis Sci. 2019;64(2):561-569.
doi pubmed - Conio M, Mangiavillano B, Caruso A, Filiberti RA, Baron TH, De Luca L, Signorelli S, et al. Covered versus uncovered self-expandable metal stent for palliation of primary malignant extrahepatic biliary strictures: a randomized multicenter study. Gastrointest Endosc. 2018;88(2):283-291.e283.
doi pubmed - Martins BC, Perez CA, Ruas JN, Bento LH, Mendonca EQ, de Paulo GA, Uemura RS, et al. Results of endoscopic biliary drainage in patients with malignant hilar stricture. Clinics (Sao Paulo). 2023;78:100153.
doi pubmed - Perdue DG, Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Overby CS, et al. Plastic versus self-expanding metallic stents for malignant hilar biliary obstruction: a prospective multicenter observational cohort study. J Clin Gastroenterol. 2008;42(9):1040-1046.
doi pubmed - Schmidt A, Riecken B, Rische S, Klinger C, Jakobs R, Bechtler M, Kahler G, et al. Wing-shaped plastic stents vs. self-expandable metal stents for palliative drainage of malignant distal biliary obstruction: a randomized multicenter study. Endoscopy. 2015;47(5):430-436.
doi pubmed - Zorron Pu L, de Moura EG, Bernardo WM, Baracat FI, Mendonca EQ, Kondo A, Luz GO, et al. Endoscopic stenting for inoperable malignant biliary obstruction: A systematic review and meta-analysis. World J Gastroenterol. 2015;21(47):13374-13385.
doi pubmed - Nakai Y, Isayama H, Kawabe T, Tsujino T, Yoshida H, Sasaki T, Tada M, et al. Efficacy and safety of metallic stents in patients with unresectable pancreatic cancer receiving gemcitabine. Pancreas. 2008;37(4):405-410.
doi pubmed - Dumonceau JM, Heresbach D, Deviere J, Costamagna G, Beilenhoff U, Riphaus A, European Society of Gastrointestinal E. Biliary stents: models and methods for endoscopic stenting. Endoscopy. 2011;43(7):617-626.
doi pubmed - Ostrowski B, Marek T, Janczewska A, Hajder N, Wiatrek A, Nowakowska-Dulawa E, Hartleb M. Performance of biliary stents in malignant biliary strictures. Pol Arch Intern Med. 2024;134(3).
doi pubmed - Wiggers JK, Groot Koerkamp B, Coelen RJ, Rauws EA, Schattner MA, Nio CY, Brown KT, et al. Preoperative biliary drainage in perihilar cholangiocarcinoma: identifying patients who require percutaneous drainage after failed endoscopic drainage. Endoscopy. 2015;47(12):1124-1131.
doi pubmed - Born P, Rosch T, Bruhl K, Sandschin W, Weigert N, Ott R, Frimberger E, et al. Long-term outcome in patients with advanced hilar bile duct tumors undergoing palliative endoscopic or percutaneous drainage. Z Gastroenterol. 2000;38(6):483-489.
doi pubmed - Isayama H, Hamada T, Yasuda I, Itoi T, Ryozawa S, Nakai Y, Kogure H, et al. TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc. 2015;27(2):259-264.
doi pubmed - Varadhachary GR, Tamm EP, Abbruzzese JL, Xiong HQ, Crane CH, Wang H, Lee JE, et al. Borderline resectable pancreatic cancer: definitions, management, and role of preoperative therapy. Ann Surg Oncol. 2006;13(8):1035-1046.
doi pubmed - Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52(2):127-149.
doi pubmed - Weston BR, Ross WA, Wolff RA, Evans D, Lee JE, Wang X, Xiao LC, et al. Rate of bilirubin regression after stenting in malignant biliary obstruction for the initiation of chemotherapy: how soon should we repeat endoscopic retrograde cholangiopancreatography? Cancer. 2008;112(11):2417-2423.
doi pubmed - Paik WH, Park YS, Hwang JH, Lee SH, Yoon CJ, Kang SG, Lee JK, et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc. 2009;69(1):55-62.
doi pubmed - Pausawasdi N, Termsinsuk P, Charatcharoenwitthaya P, Limsrivilai J, Kaosombatwattana U. Development and validation of a risk score for predicting clinical success after endobiliary stenting for malignant biliary obstruction. PLoS One. 2022;17(8):e0272918.
doi pubmed - So H, Oh CH, Song TJ, Ko SW, Hwang JS, Oh D, Park DH, et al. Predictors of stent dysfunction in patients with bilateral metal stents for malignant hilar obstruction. PLoS One. 2021;16(3):e0249096.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Gastroenterology Research is published by Elmer Press Inc.