Impact of Hospital Teaching Status on Outcomes of Acute Cholangitis: A Propensity-Matched Analysis of Hospitalizations in the United States
DOI:
https://doi.org/10.14740/gr2038Keywords:
Acute cholangitis, Teaching hospitals, Outcomes, Hospital mortality, Hospital charges, Hospital length of stay, National Inpatient Sample databaseAbstract
Background: Acute cholangitis (AC) is a serious condition caused by partial or complete obstruction of the common bile duct (CBD), leading to biliary tract infection. We aimed to evaluate whether teaching hospitals with trainees and non-teaching hospitals impact the outcome of AC in the United States.
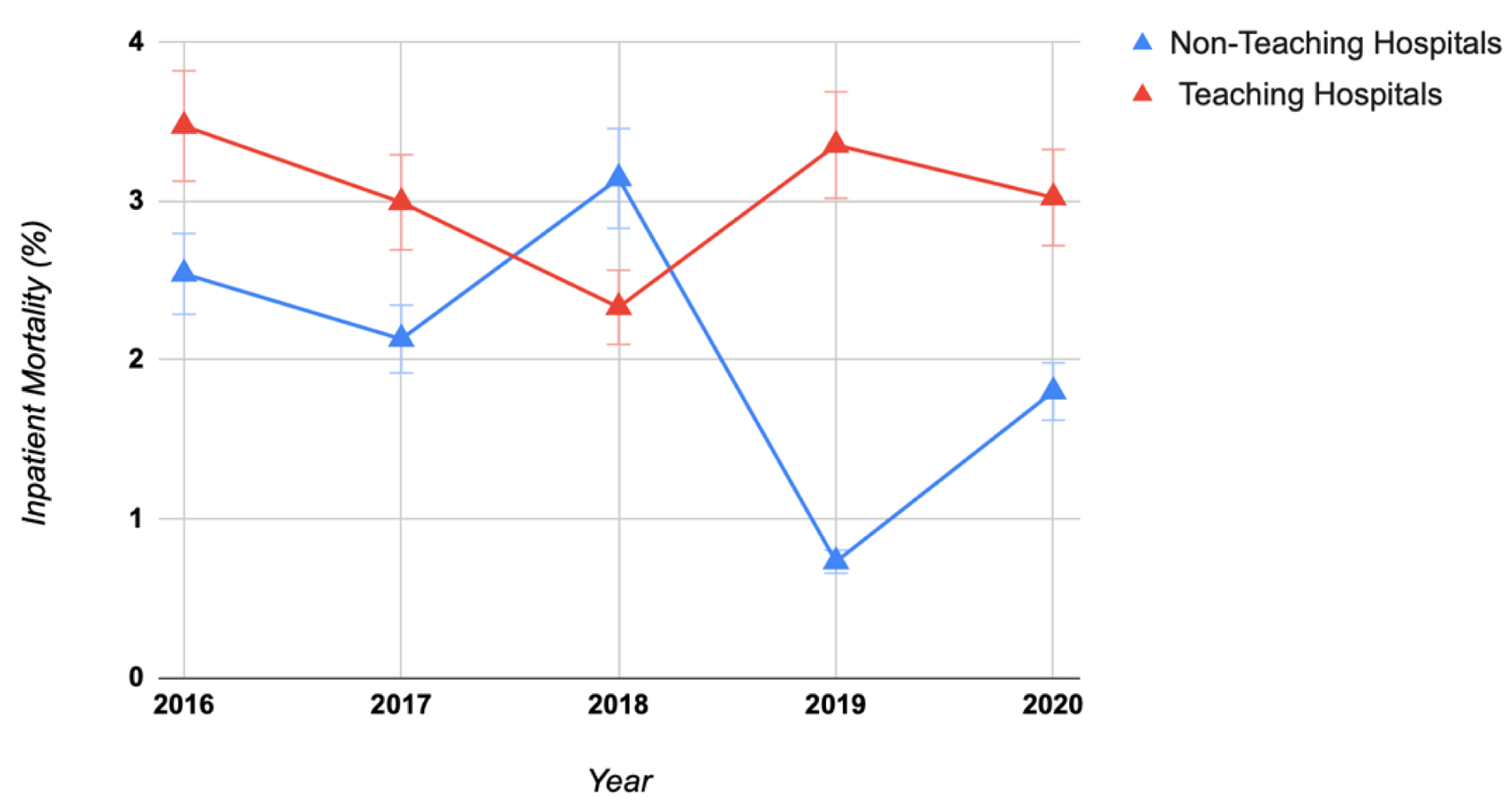
Methods: This study utilized the National Inpatient Sample database to analyze adult hospitalizations (> 18 years old) with a primary diagnosis of AC in the USA from 2016 to 2020. A multivariate logistic regression along with Chi-square and t-tests was performed using SAS 9.4 software to analyze inpatient AC-associated mortality, inflation-adjusted total hospitalization costs (THC), and length of stay (LOS) in US teaching and non-teaching hospitals during the study period.
Results: This study included a total of 30,300 patients, out of whom 23,535 (about 78%) were managed in teaching hospitals and 6,765 (about 22%) were managed in non-teaching hospitals. Primary outcomes showed a significant increase in mortality for patients managed in teaching hospitals (2.77% vs. 2.08%, P = 0.01) in comparison to non-teaching hospitals, hospital LOS was slightly higher in teaching hospitals (5 days (interquartile range (IQR): 3 - 6) vs. 4 days (IQR: 3 - 8)) and so did hospital cost ($15,259 vs. $14,506) in comparison to non-teaching hospitals. Secondary outcomes showed that patients in teaching hospitals had higher incidence of septic shock (16.06% vs. 12.53%, P < 0.0001), intensive care unit (ICU) admissions (6.61% vs. 5.07%, P = 0.0002), and intubation (5.30% vs. 3.46%, P < 0.0001) in comparison to non-teaching hospitals.
Conclusion: Our study found higher mortality rates for AC patients in teaching hospitals compared to non-teaching hospitals. Teaching hospitals also had higher rates of septic shock, ICU admission, and intubation, with no difference in endoscopic retrograde cholangiopancreatography (ERCP) use. These differences could be due to several factors, such as greater resident and fellow autonomy in teaching hospitals and a potentially more proactive approach by physicians in non-teaching hospitals. Additionally, teaching hospitals often manage more complex, higher-acuity cases, which could contribute to worse outcomes.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.