Comparison of Prophylactic Transcatheter Arterial Embolization and Standard Therapy in High-Risk Non-Variceal Upper Gastrointestinal Bleeding: A Meta-Analysis
DOI:
https://doi.org/10.14740/gr2041Keywords:
Prophylactic transcatheter arterial embolization, Non-variceal upper gastrointestinal bleeding, Rebleeding, Mortality, Endoscopic hemostasis, High-risk patients, Meta-analysis/systematic review, Adverse events/complicationsAbstract
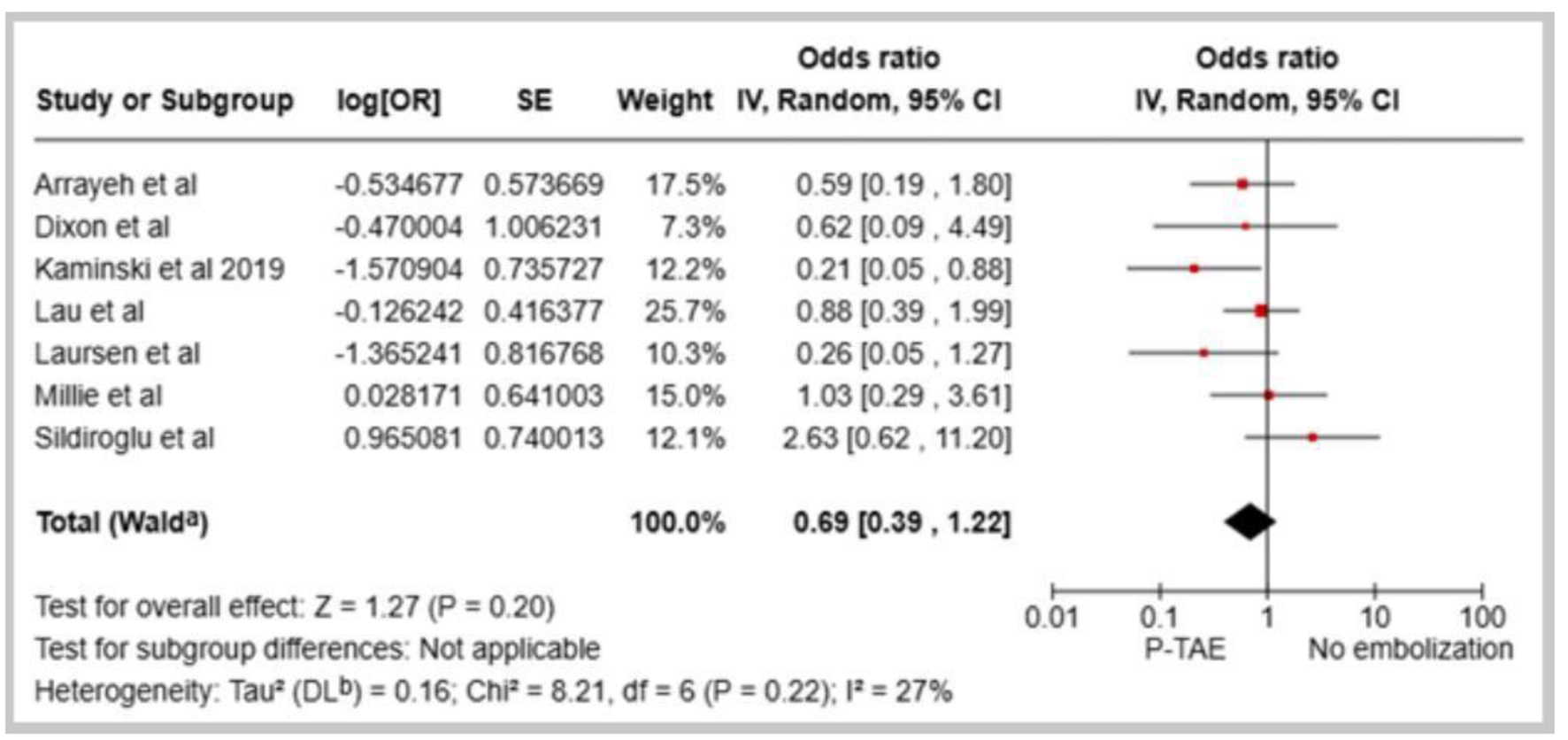
Background: Rebleeding is a major challenge and a serious complication of non-variceal upper gastrointestinal bleeding (NVUGIB). Prophylactic transcatheter arterial embolization (P-TAE) has emerged as a potential management strategy for high-risk cases. This study aimed to evaluate the efficacy and safety of P-TAE compared with no embolization (NE) in the absence of angiographic evidence of bleeding or therapeutic arterial embolization (TAE).
Methods: The study systematically searched Medline and Embase databases from inception until November 15, 2024. The primary outcome was the overall rebleeding rate, while secondary outcomes included mortality, need for additional interventions, transfusion requirements, hospital/intensive care unit (ICU) stay, and procedure-related adverse events.
Results: The meta-analysis included 10 studies with a total population of 1,253 patients. Compared to NE, the pooled data indicated that P-TAE was not associated with significantly reduced rates of rebleeding (odds ratio (OR): 0.69, 95% confidence interval (CI): 0.39 - 1.22, P = 0.20) or all-cause mortality (OR: 0.70, 95% CI: 0.40 - 1.23). Although P-TAE trended towards lower rates of repeat interventions, blood transfusions, and shorter hospital stays, these differences were not statistically significant. Conversely, P-TAE and TAE had similar rates of rebleeding (OR: 1.08, 95% CI: 0.70 - 1.68, P = 0.05) and all-cause mortality (OR: 0.72, 95% CI: 0.34 - 1.51, P = 0.39). The analysis found no significant differences in adverse events or the need for repeat procedures between the two embolization approaches.
Conclusion: This review suggests that P-TAE may not significantly reduce rebleeding or mortality compared with standard therapy for high-risk NVUGIB. However, the current findings remain inconclusive, and further comprehensive research with larger sample sizes is required to conclusively substantiate these observations.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.